DRESS Syndrome: Causes, Symptoms, and Medications That Trigger It
When your body overreacts to a medication, it can trigger something called DRESS syndrome, a life-threatening drug-induced hypersensitivity reaction that affects the skin, organs, and immune system. Also known as drug reaction with eosinophilia and systemic symptoms, it doesn’t just cause a rash—it can shut down your liver, kidneys, or lungs if ignored. This isn’t a common allergy like a peanut reaction. It’s slower, sneakier, and often shows up weeks after you start a new drug.
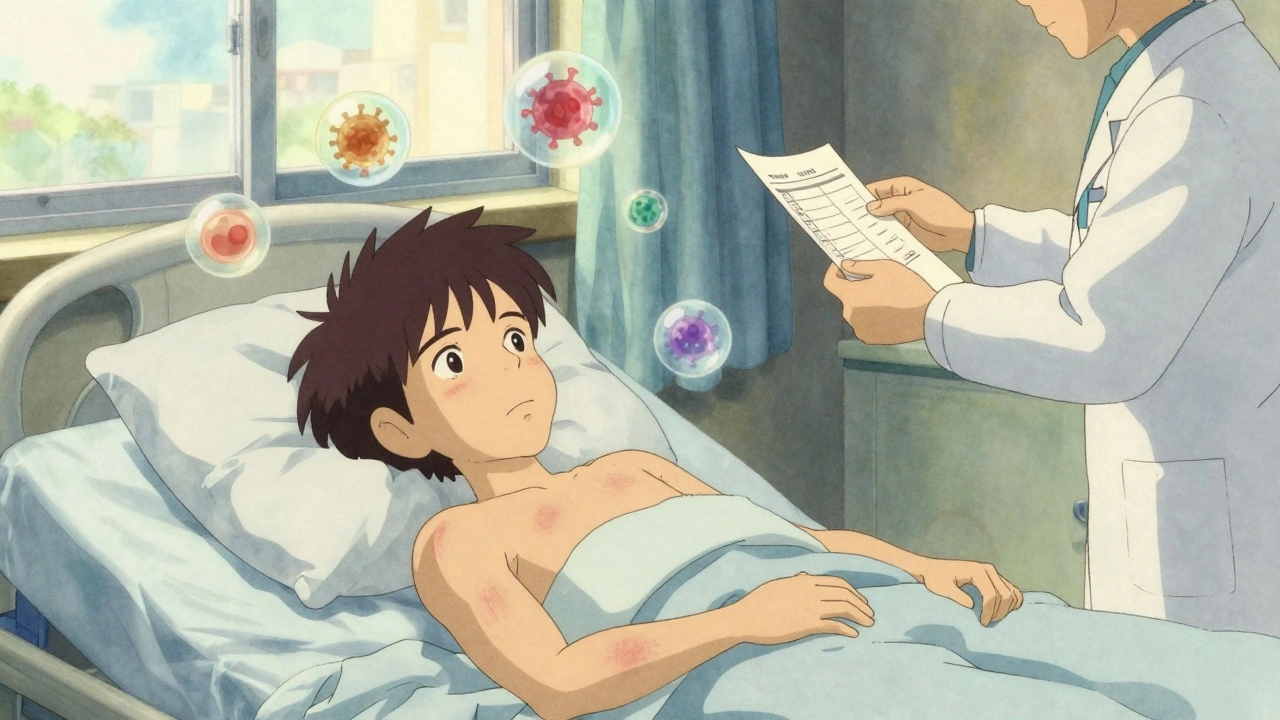
DRESS syndrome usually shows up 2 to 8 weeks after taking the offending medicine. Common triggers include anticonvulsants, drugs like carbamazepine, phenytoin, and lamotrigine used for seizures and nerve pain, allopurinol, a gout medication that’s one of the top culprits, and some antibiotics or antivirals. You might notice a fever, swollen lymph nodes, and a widespread red rash that feels like a bad sunburn. Blood tests often show high eosinophils—white blood cells that scream "immune system on fire." Liver damage is common, and in severe cases, the kidneys or heart get involved too.
What makes DRESS syndrome dangerous is how easily it’s mistaken for something else. Doctors might think it’s a viral infection, a skin condition, or even a side effect you just have to live with. But if you’ve started a new drug and suddenly feel awful—fever, rash, swollen glands—it’s not just bad luck. It’s a medical emergency. Stopping the drug right away is step one. Delaying treatment increases the risk of long-term organ damage or death.
People who carry certain genes, like HLA-B*58:01, are at higher risk when taking allopurinol. That’s why some doctors test for it before prescribing. But you don’t need a genetic test to know your body’s warning signs. If you’ve had DRESS before, avoid the same drug—and tell every new doctor. Even a small dose can bring it back.
The posts below cover real cases and critical details: how DRESS links to other drug reactions, which medications are most likely to cause it, what blood tests reveal, and how to tell the difference between a harmless rash and a life-threatening one. You’ll also find advice on what to do if you suspect a reaction, how to talk to your pharmacist about risks, and how to avoid dangerous combinations with other meds like those for blood pressure or seizures. This isn’t theoretical. These are stories from people who lived through it—and what they wish they’d known sooner.