Drug Hypersensitivity: Signs, Risks, and What to Do When Your Body Reacts
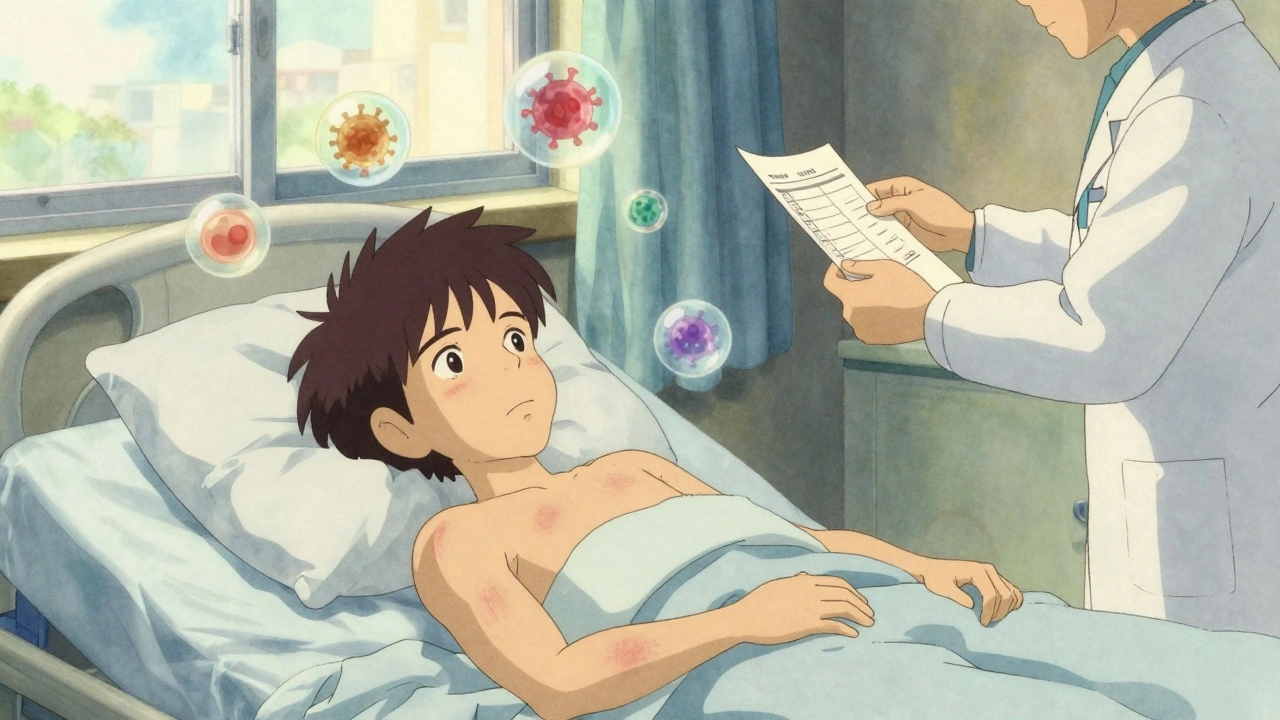
When your body treats a medication like a foreign invader, that’s drug hypersensitivity, an immune system overreaction to a drug that isn’t caused by the drug’s intended effect. Also known as adverse drug reaction, it’s not just a rash or an upset stomach—it can mean trouble breathing, swelling, organ damage, or even death. Unlike side effects, which are predictable and dose-related, drug hypersensitivity is unpredictable and can happen even with a tiny amount of medicine you’ve taken before without issue.
This isn’t rare. Studies show up to 1 in 5 people will experience some form of drug hypersensitivity in their lifetime. Some medications are far more likely to trigger it—antibiotics like penicillin, seizure drugs like carbamazepine, and painkillers like sulfa drugs are common culprits. If you’ve ever broken out in hives after taking an antibiotic, or felt dizzy and nauseous right after a new prescription, that might’ve been your immune system sounding the alarm. And it’s not just about the drug itself—drug interaction, when two or more medications mix in ways that change how your body handles them can turn a safe drug into a dangerous one. Grapefruit juice with blood pressure meds, or NSAIDs with blood thinners, can amplify risks you never saw coming.
What makes this even trickier is that symptoms can show up hours, days, or even weeks after you start a new drug. A mild rash might seem harmless, but it could be the first sign of something like Stevens-Johnson syndrome—a severe skin reaction that needs emergency care. If you’ve ever switched from a brand-name drug to a generic medication, a version of a drug made after the patent expires, often cheaper but sometimes triggering different reactions and noticed new side effects, you’re not alone. Many people report changes in how they feel after the switch, even if the active ingredient is the same. That’s because fillers, dyes, or manufacturing differences can trigger hypersensitivity in sensitive individuals.
Knowing your history matters. If you’ve had a reaction to one drug, you’re more likely to react to others in the same class. Penicillin allergy? You might also react to amoxicillin. Sulfa allergy? Avoid certain diuretics and diabetes meds. Keeping a simple list of drugs that caused problems—not just the name, but what happened—can save your life. And if you’re on multiple meds, like many seniors or people with chronic conditions, the chances of a hidden interaction go up fast. That’s why pharmacists are such a vital part of your care team—they spot these risks before you even walk out the door.
There’s no single test for drug hypersensitivity. Doctors often rely on your symptoms, timing, and elimination. If you stop the drug and the reaction fades, that’s a strong clue. But if you’ve ever had a severe reaction, you may need to carry an alert card or wear a medical bracelet. Emergency treatment usually means stopping the drug, using antihistamines or steroids, and in worst cases, epinephrine. The key is catching it early.
Below, you’ll find real stories and science-backed guides on what to watch for, which drugs carry the highest risk, how to tell if it’s just a side effect or something serious, and what to do if you or someone you love reacts unexpectedly. These aren’t theory pieces—they’re practical, urgent, and written for people who’ve been there.