DRESS Diagnosis: Understanding Drug-Induced Autoimmune Reactions and What to Do Next
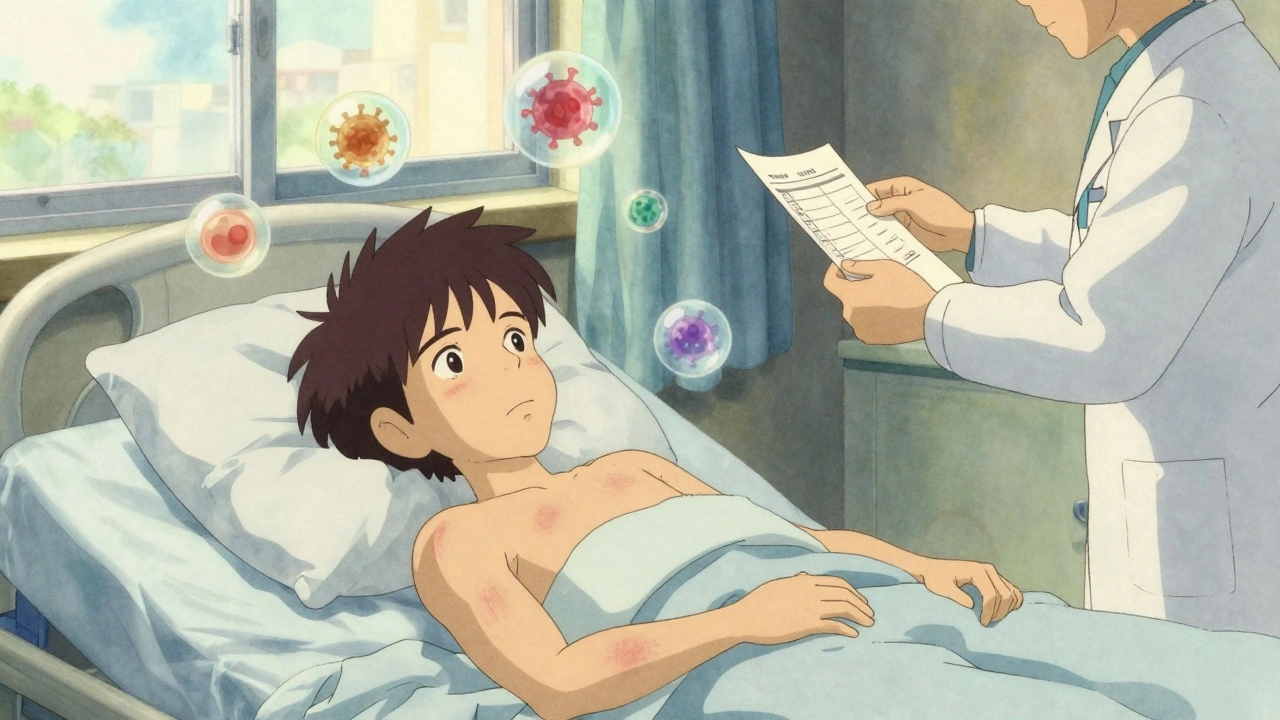
When your body reacts to a medication like it’s under attack, it’s not just a rash—it could be DRESS diagnosis, a severe, delayed immune reaction to certain drugs that affects multiple organs. Also known as Drug Reaction with Eosinophilia and Systemic Symptoms, this condition doesn’t show up right away. It can take weeks to develop after starting a new medicine, and if ignored, it can lead to liver failure, kidney damage, or even death. Unlike a simple allergic reaction, DRESS isn’t just skin deep. It triggers your immune system to go haywire, flooding your blood with eosinophils—white blood cells that normally fight parasites but here, mistakenly target your own organs.
What drugs cause this? Common culprits include anticonvulsants, medications like carbamazepine, phenytoin, and lamotrigine used for seizures and mood disorders, antibiotics, especially sulfonamides and minocycline, and even some gout treatments like allopurinol. These aren’t rare drugs—they’re prescribed millions of times a year. But only a small fraction of people develop DRESS. The risk isn’t random. Genetics play a role. Some people carry specific genes (like HLA-B*58:01) that make them far more likely to react badly. That’s why one person gets a mild rash, and another ends up in the ICU.
Here’s what to watch for: a fever that won’t quit, swollen lymph nodes, a spreading red rash, and unusual fatigue. Then come the internal signs—elevated liver enzymes, kidney trouble, or lung inflammation. Blood tests showing high eosinophils are a red flag. Many doctors miss it because the symptoms look like infections or other autoimmune diseases. That’s why timing matters. If you started a new medication 2 to 8 weeks ago and now feel worse, don’t assume it’s just a virus. Ask your doctor about DRESS diagnosis. Stopping the drug early can stop the damage. Waiting too long? That’s when organs start failing.
The good news? Once you identify the trigger and get off the drug, most people recover—though it can take months. Some need steroids to calm the immune system. Others need hospital care. There’s no cure, but there’s a clear path: stop the drug, monitor closely, treat symptoms, and never restart it. And if you’ve had DRESS once, you’re at risk for it again with similar drugs. That’s why knowing your history matters.
Below, you’ll find real-world stories and medical insights from people who’ve been through this—and the doctors who’ve learned how to spot it before it’s too late. From medication switches that saved lives to the hidden risks in common prescriptions, these posts give you the facts you need to protect yourself or someone you care about.