When you take a new medication, you might worry about side effects. But not every bad reaction is a side effect-some are drug allergies. These aren’t just unpleasant surprises; they’re your immune system overreacting to something in the medicine. And while most drug reactions aren’t allergic, the ones that are can turn dangerous fast. Knowing the difference could save your life.
What Makes a Drug Allergy Different?
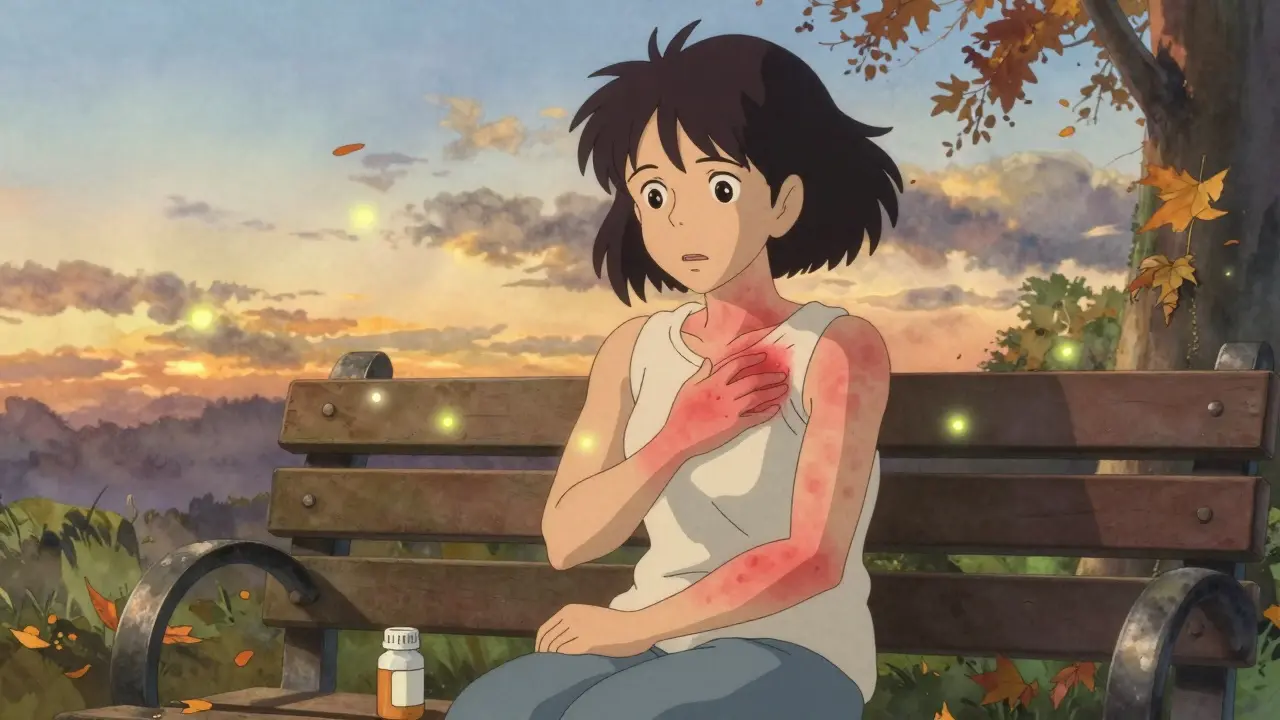
A drug allergy isn’t the same as a stomachache from antibiotics or dizziness from blood pressure pills. Those are side effects-expected, pharmacological reactions. A true drug allergy means your immune system sees the drug as an invader and attacks it. That’s why two people can take the same pill and one gets a rash while the other feels fine. It’s not about the drug being ‘strong’ or ‘weak.’ It’s about your body’s unique response.The most common sign? A skin rash. But that’s just the start. Drug allergies can show up in hours-or weeks. Some reactions are mild. Others? They can shut down your lungs, drop your blood pressure, or peel your skin off. That’s why timing and symptoms matter more than you think.
Common Signs of a Drug Allergy
Here’s what to watch for, broken down by how soon symptoms appear:
- Within minutes to an hour: Hives (red, itchy welts), swelling of the lips, tongue, or throat, wheezing, trouble breathing, vomiting, dizziness, or a sudden drop in blood pressure. This is a red flag for anaphylaxis-a life-threatening reaction that hits multiple systems at once. If you have a rash and trouble breathing, don’t wait. Call 911.
- Hours to days later: A widespread, flat, red rash that itches. This is often called a drug exanthem. It usually shows up 5 to 14 days after starting the medicine. You might feel fine otherwise-no fever, no swelling. Still, stop the drug and call your doctor.
- One to three weeks later: Fever, swollen lymph nodes, joint pain, and a rash that looks like hives or red patches. This could be serum sickness-like reaction. It’s rare, but it happens with antibiotics like cefaclor or minocycline.
- Three weeks or more: A rash that spreads, blisters, or peels. If your mouth, eyes, or genitals are also affected, this could be Stevens-Johnson Syndrome (SJS) or Toxic Epidermal Necrolysis (TEN). These are medical emergencies. Skin can detach like a severe burn. Survival depends on quick hospital care.
Other signs to never ignore: high fever without infection, swollen glands, liver pain (right side of your belly), or unexplained bruising. These could point to DRESS syndrome-a delayed reaction that can damage your organs. It’s rare, but deadly if missed.
When to Go to the Emergency Room
You don’t need to guess. If you have any two of these symptoms together, get help immediately:
- Difficulty breathing or wheezing
- Swelling in your throat, tongue, or face
- Feeling faint, dizzy, or passing out
- Rapid heartbeat or cold, clammy skin
- Severe rash with blistering or peeling skin
- Nausea, vomiting, or diarrhea along with a rash
This isn’t a ‘wait and see’ situation. Anaphylaxis can kill in under 10 minutes. Even if you’ve had mild reactions before, the next one can be worse. Never assume you’re ‘safe’ just because you’ve taken the drug before. Allergies can develop at any time.

What You Should Do After a Reaction
If you survive a serious reaction, your next step isn’t just to avoid the drug. It’s to get properly diagnosed.
Most people who say they’re allergic to penicillin aren’t. Studies show over 90% of them can take it safely after testing. Yet, because they’re labeled allergic, doctors give them stronger, costlier antibiotics that raise the risk of dangerous infections like C. diff. That’s why mislabeling isn’t just inconvenient-it’s a public health problem.
Here’s what to do next:
- Stop the drug. Don’t wait for a doctor’s permission. If you suspect an allergic reaction, stop taking it.
- Take photos. If you can’t get to a doctor right away, snap clear pictures of the rash, swelling, or blisters. Visuals help doctors more than descriptions.
- Write down details. What was the drug? When did you take it? When did symptoms start? What did they feel like? Include any other meds or supplements you were on.
- See an allergist. Your regular doctor might not know how to test for drug allergies. An allergist or immunologist has the right tools. For penicillin, they’ll do skin tests and possibly an oral challenge under supervision. For other drugs, they might use blood tests or carefully controlled doses to see if you react.
Don’t rely on old labels. If you were told you’re allergic to penicillin as a kid, get tested now. You might be able to use it safely.
Why Diagnosis Matters More Than You Think
Doctors often guess. They see a rash, assume it’s allergic, and write ‘penicillin allergy’ in your chart. That label sticks forever. But without testing, you’re stuck with less effective, more expensive, and riskier alternatives.
Penicillin is the most commonly mislabeled drug allergy. But it’s not the only one. Sulfa drugs, NSAIDs like ibuprofen, and certain seizure meds can also trigger real allergies. And if you’ve had a severe reaction to one drug, you’re at higher risk for reactions to others.
There’s no blood test for most drug allergies. Skin tests only exist for penicillin and a few others. That’s why history matters. Your detailed story-when the reaction happened, what it looked like, how fast it came on-is the most important diagnostic tool.

How to Protect Yourself Going Forward
Once you know what you’re allergic to, take action:
- Wear a medical alert bracelet or necklace listing your drug allergies.
- Keep a written list in your phone and wallet. Include the drug name and what happened.
- Always tell every doctor, dentist, and pharmacist about your allergies-even if you think they don’t matter.
- Ask if a drug you’re prescribed is in the same class as one you reacted to. For example, if you’re allergic to amoxicillin, you might also react to other penicillin-based drugs.
- Don’t assume over-the-counter meds are safe. Some painkillers and cold remedies contain ingredients you’re allergic to.
And if you ever feel unsure-call your doctor. Don’t risk it. A mild rash today could be a warning sign for something worse tomorrow.
Final Thought: Trust Your Body, But Verify
Drug allergies are rare-but their consequences are real. Most people who think they’re allergic aren’t. And most people who are allergic don’t know it. The key isn’t fear. It’s awareness. Pay attention to your body. Know the signs. Act fast when needed. And don’t let a misdiagnosis limit your care.
Your health isn’t something to guess about. It’s something to understand.
How do I know if my rash is from a drug allergy or just a side effect?
A side effect is usually predictable and doesn’t involve your immune system-like nausea from antibiotics or dizziness from blood pressure meds. A drug allergy triggers your immune system and often includes itching, hives, swelling, or trouble breathing. If your rash is accompanied by any of those, especially if it appeared after starting a new drug, it’s likely allergic. Side effects don’t typically cause swelling or breathing issues.
Can I outgrow a drug allergy?
Yes, especially with penicillin. Many people lose their allergy over time. Studies show that up to 80% of people who were once allergic to penicillin can tolerate it again after 10 years. That’s why it’s critical to get tested if you were labeled allergic years ago. You might be able to safely use a more effective, less expensive antibiotic.
Is there a blood test for drug allergies?
There’s one blood test that can help for severe delayed reactions like DRESS syndrome-it checks for high eosinophils and other markers. But for most drug allergies, including penicillin, there’s no reliable blood test. Skin testing is the gold standard for penicillin. For others, diagnosis relies on your history, physical exam, and sometimes a controlled drug challenge under medical supervision.
What if I had a reaction but didn’t see a doctor?
If you had a mild rash that went away on its own, still document it. Take photos and write down the drug name and when you took it. Even if it seems minor, it could be a warning sign. If you had swelling, trouble breathing, or blisters, you need to see an allergist. Don’t assume it won’t happen again. Reactions can get worse with each exposure.
Can I take a similar drug if I’m allergic to one?
Not without testing. Drugs in the same class (like different penicillins or sulfa drugs) often cross-react. But not always. For example, some people allergic to one antibiotic in the penicillin family can tolerate another. Only an allergist can safely determine this through testing. Never guess-this could be life-threatening.
Are there any drugs I should avoid if I’ve had a drug allergy before?
Yes. If you’ve had a severe reaction to one drug, you’re at higher risk for reactions to others, especially if they’re chemically similar. Common triggers include penicillin, sulfa drugs, NSAIDs like ibuprofen, and certain seizure medications. But the biggest risk is mislabeling. If you’ve been told you’re allergic to penicillin, get tested before avoiding all penicillin-class drugs. You might be able to use them safely.

man i had this weird rash after amoxicillin back in uni-thought it was just heat or somethin. turned out it was a delayed hypersensitivity. docs just shrugged and said 'probably allergy' but never tested me. now i avoid all penicillins like plague. but honestly? i think most people just get labeled allergic bc no one wants to do the work. the real issue is the healthcare system doesn't care enough to follow up. we're just handed labels and told to live with 'em.
these drug allergies are just big pharma lies to sell you more expensive pills. if your body reacts, it means you're too weak. in india we take 5 medicines at once and still go to work. you think your skin rash is special? get real. stop being soft.
the article is accurate but overly verbose. 80% of it could be condensed into a bullet list. also, no mention of cross-reactivity with cephalosporins in penicillin-allergic patients. that’s a major gap.
OMG i had SJS after taking sulfa! it was the worst thing ever. my skin peeled off like a banana. i took pics and went to ER right away. they saved me. but now my dr keeps forgettin i’m allergic and prescribes Bactrim. i have to yell EVERY TIME. pls just put it in your notes!!
what’s fascinating is how much we rely on anecdotal history over science here. we don’t have good biomarkers for most drug allergies, so we’re stuck with this fragile, subjective system where your memory of a rash 15 years ago dictates your treatment for life. it’s like diagnosing diabetes based on how you felt once at a family BBQ. we need better tools-but until then, documenting everything matters more than we realize.
THIS. This is the kind of info every person needs. I used to think penicillin allergy was permanent-until I got tested at 32. Turns out I was never allergic. I’ve been on cheaper, better meds since. Saved my family thousands. If you’ve been told you’re allergic-GET TESTED. It’s not scary, it’s life-changing. 💪❤️
you think the system cares about your skin rash? no. they care about liability. if you die from anaphylaxis, they get sued. if you get a rash and live? they chalk it up to 'possible allergy' and move on. the real tragedy isn’t the drug-it’s the bureaucracy that turns medical intuition into a permanent prison sentence. your body isn’t broken. the system is.
Thank you for this comprehensive overview. It is imperative that patients document reactions accurately and consult allergists for confirmation. Mislabeling can lead to inappropriate antibiotic use and increased antimicrobial resistance. Professional evaluation is strongly advised.