Therapeutic Drug Monitoring: What It Is and Why It Matters for Your Medications
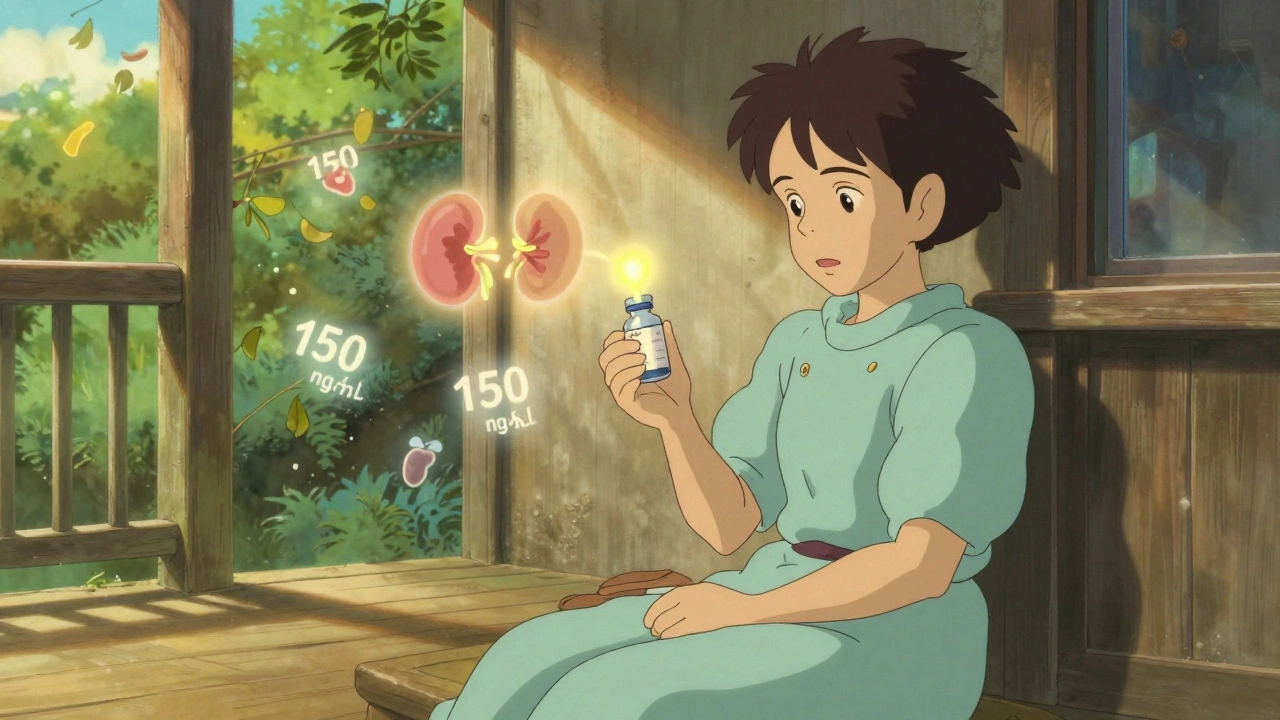
When you take certain medications, it’s not just about the dose on the label—it’s about what’s actually happening in your body. Therapeutic drug monitoring, the process of measuring the concentration of a drug in your bloodstream to ensure it’s in the right range. Also known as TDM, it’s a quiet but powerful tool that keeps powerful drugs from turning harmful. This isn’t for every pill you take. It’s reserved for drugs where even a small change in blood level can mean the difference between healing and harm—like heart meds, seizure drugs, or antibiotics used for serious infections.
Why does this matter? Because your body processes drugs differently than your neighbor’s. Age, liver function, kidney health, and even what you eat can change how much of a drug stays in your system. For example, blood tests for meds, routine lab checks that track how much drug is circulating, help doctors spot if you’re underdosed (and not getting relief) or overdosed (and risking toxicity). One study found that nearly 1 in 5 patients on long-term antibiotics had unsafe levels—until their doses were adjusted using TDM. That’s not rare. It’s common enough that hospitals run these tests daily.
It’s not just about safety. It’s about effectiveness. If your seizure medication isn’t at the right level, you could have a breakthrough seizure. If your transplant drug is too low, your body might reject the new organ. Too high, and your kidneys or nerves could be damaged. That’s why medication safety, the practice of ensuring drugs work without causing harm isn’t just about following instructions—it’s about knowing what’s in your blood. And that’s where TDM steps in. It turns guesswork into data.
Some of the most common drugs tracked this way include digoxin for heart failure, vancomycin for tough infections, lithium for bipolar disorder, and cyclosporine for transplant patients. But it’s not just about those. Even drugs like antidepressants and anticonvulsants can benefit from monitoring, especially when side effects show up or the medicine stops working. And when you’re on multiple meds, drug interactions, when one medicine changes how another behaves in your body can throw off your levels without you even noticing.
You won’t always know you need it. Your doctor won’t always bring it up. But if you’re on a drug with a narrow window between helpful and harmful—if you’ve had side effects, if your condition isn’t improving, or if you’ve had recent changes in health—ask about TDM. It’s not a luxury. It’s a basic check, like a tire pressure light in your car. Only instead of a flat tire, you’re avoiding organ damage or treatment failure.
Below, you’ll find real-world stories and science-backed guides on how drugs behave in the body, when to question your dose, how labs interpret results, and what to do if your meds suddenly stop working. These aren’t abstract theories. They’re the kind of details that keep people out of the ER—and help them live better every day.