Cyclosporine Safety Calculator
Cyclosporine Safety Calculator
Check if your cyclosporine level is within the safe therapeutic window based on kidney function. This tool helps you determine if your levels are safe or if you should contact your healthcare provider.
When you take cyclosporine after a transplant, your body needs just the right amount-too little and your immune system attacks the new organ; too much and your kidneys start to fail. This isn’t a guesswork situation. It’s a tightrope walk measured in nanograms per milliliter. For over 40 years, cyclosporine has kept transplanted kidneys, hearts, and livers alive, but its dark side-nephrotoxicity-is why so many patients lose their grafts years later. The good news? You can prevent most of it. The key is knowing cyclosporine nephrotoxicity isn’t random. It’s predictable. And it’s monitorable.
What Makes Cyclosporine So Dangerous for Kidneys
Cyclosporine doesn’t just suppress your immune system. It also tightens the blood vessels inside your kidneys. This reduces blood flow, which sounds harmless until your kidneys start working harder to filter waste. Over time, this causes scarring in the tiny tubes and arteries. The damage starts quietly-no pain, no swelling. By the time creatinine rises, you’ve already lost 20-30% of kidney function.
Studies show that 30-50% of long-term kidney transplant failures are linked to cyclosporine toxicity. That’s not because the drug is broken. It’s because it’s used without precision. The drug’s therapeutic window is razor-thin: the difference between a safe level and a toxic one is smaller than the margin of error in some lab tests.
How to Measure Cyclosporine Correctly
Not all blood tests for cyclosporine are created equal. Back in 2002, 85% of labs used immunoassays-fast, cheap, and widely available. But here’s the catch: these tests can’t tell the difference between cyclosporine and its metabolites. That means if your body breaks down the drug into similar-looking compounds, the machine might read your level as 250 ng/mL when it’s really 180 ng/mL. That’s a 40% overestimate. That’s dangerous.
Today, the gold standard is LC-MS/MS-liquid chromatography-tandem mass spectrometry. It’s specific. It’s accurate. It detects levels as low as 5 ng/mL. By 2021, 92% of U.S. transplant centers switched to this method. If your lab still uses immunoassays, ask why. Accuracy isn’t optional when your kidneys are on the line.
And don’t forget the tube. Blood for cyclosporine must go into EDTA tubes-purple top. Not serum separator tubes (red or gold). Using the wrong tube can falsely raise levels by 15-20%. That’s enough to trigger a dangerous dose reduction.
When to Draw Blood: Trough vs. C2 Monitoring
For decades, doctors checked cyclosporine levels right before your next dose-the “trough” or C0 level. But here’s what they didn’t know: that number doesn’t reflect how much drug your body actually absorbed over the day.
Now, C2 monitoring-measuring the level two hours after your dose-is the new standard. Why? Because C2 correlates 87% with total drug exposure over 24 hours. Trough levels only correlate at 63%. That’s a huge gap.
Centers using C2 monitoring saw a 22.4% drop in nephrotoxicity between 2018 and 2022. That’s not a small win. That’s life-saving. And it’s not complicated: just draw blood two hours after you swallow your pill. No fasting. No special prep. Just timing.
But here’s the catch: you have to be consistent. If you take your pill at 8 a.m. one day and 9 a.m. the next, your C2 reading changes. Set an alarm. Stick to the schedule. Your kidneys will thank you.
What Kidney Numbers to Watch Every Week
Don’t just rely on cyclosporine levels. Your kidneys send signals. Learn to read them.
- Serum creatinine: Keep it under 1.5 mg/dL. If it climbs above 1.8 mg/dL and stays there for two weeks, your doctor needs to act.
- BUN-to-creatinine ratio: Should be under 20:1. A higher ratio suggests dehydration or reduced kidney blood flow-both worsen cyclosporine damage.
- Blood pressure: Target under 130/80 mmHg. High blood pressure speeds up kidney scarring. You may need an ACE inhibitor or ARB, even if your pressure seems “normal.”
- Magnesium: Cyclosporine makes you lose magnesium. Normal range is 1.7-2.2 mg/dL. If you’re below 1.5, you’ll feel weak, shaky, or get muscle cramps. Supplementing helps.
- Uric acid: Cyclosporine raises it. Not everyone needs to track this, but if you get gout attacks or kidney stones, it’s worth checking.
Track these numbers monthly at first. Then every 2-3 months if you’re stable. Don’t wait for symptoms. By then, it’s too late.
Drug Interactions That Can Kill Your Kidneys
Cyclosporine is processed by your liver using an enzyme called CYP3A4. Many common drugs mess with this system.
- Antifungals like ketoconazole: Can spike cyclosporine levels by 30-50%. Avoid if possible. If you need it, your dose must be cut by half-and your levels checked within 48 hours.
- Antibiotics like rifampin: Can slash cyclosporine levels by 40-60%. You might reject your transplant without realizing why.
- St. John’s Wort: A popular herbal supplement. It lowers cyclosporine levels. Stop it. Now.
- Grapefruit juice: One glass can raise cyclosporine levels by 25%. Don’t drink it. Ever.
Always tell every doctor-dentist, pharmacist, even your chiropractor-that you’re on cyclosporine. Even a simple antibiotic for a sinus infection can throw your levels off.
Genetics Play a Bigger Role Than You Think
Not everyone breaks down cyclosporine the same way. Your genes matter.
About 15% of people have a genetic variant called CYP3A5*1. These are “extensive metabolizers.” Their bodies clear cyclosporine fast. If they get the standard dose, they’re underdosed. Their rejection risk goes up.
Starting in 2023, KDIGO guidelines recommend testing for CYP3A5 status before starting cyclosporine. If you’re an extensive metabolizer, you may need 30-40% more drug to reach safe levels. No one should be dosed blindly anymore.
What Happens If You Don’t Monitor?
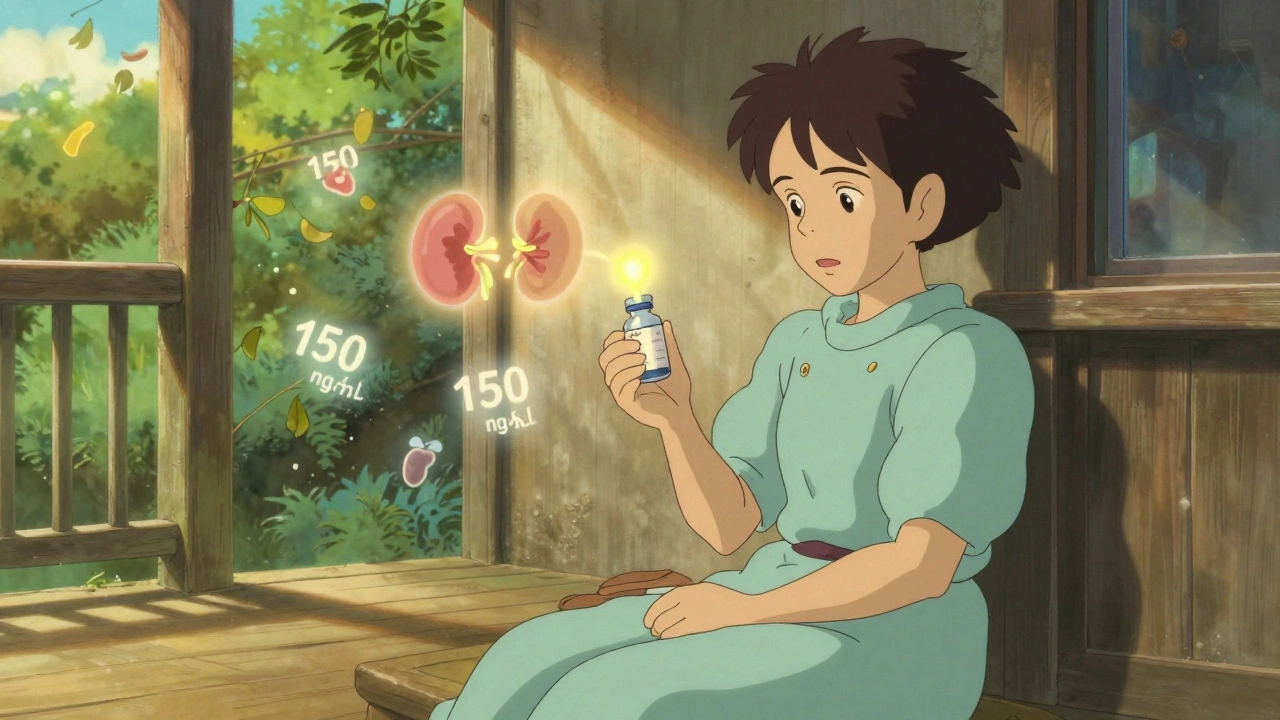
Let’s say you skip blood tests for three months. Your creatinine creeps up from 1.2 to 1.9. Your blood pressure rises. You feel tired. You blame stress. But your cyclosporine level? It’s 320 ng/mL-way above the 150 ng/mL target for year two post-transplant.
At this point, your kidneys are already scarred. The damage is irreversible. Even if you lower the dose now, your function won’t bounce back. You might need dialysis. Or another transplant.
That’s why monitoring isn’t just “recommended.” It’s non-negotiable. Every transplant center that follows strict protocols sees 50% fewer kidney failures from cyclosporine toxicity.
What’s Next? The Future of Monitoring
Point-of-care devices are coming. By late 2025, FDA-approved machines may let you check your cyclosporine level at home with a finger-prick blood sample-results in under 15 minutes. AI tools are already being tested to predict your ideal dose based on your weight, age, liver function, and genetics. These won’t replace labs, but they’ll make monitoring less burdensome.
For now, stick to the basics: accurate blood tests, consistent timing, awareness of drug interactions, and tracking your kidney numbers. Don’t wait for your doctor to catch something. Be the one who notices the trend.
What to Do If Your Levels Are Too High
If your cyclosporine level is above target and your creatinine is rising:
- Don’t panic. Don’t skip your next dose.
- Call your transplant team immediately. Don’t wait for your next appointment.
- Review all medications and supplements you’ve taken in the past week.
- Get a C2 level if you’ve only been doing C0.
- Expect a 20-30% dose reduction, followed by retesting in 5-7 days.
Reversing early toxicity works. Studies show kidney function improves in 70% of patients if the dose is lowered within three months of the first sign of damage.
Can cyclosporine nephrotoxicity be reversed?
Yes, if caught early. If kidney function declines due to high cyclosporine levels and the dose is reduced within 3 months, up to 70% of patients see improvement in creatinine and blood flow. But after 6-12 months of sustained toxicity, scarring becomes permanent. Early detection is everything.
How often should cyclosporine levels be checked?
In the first month after transplant, check twice weekly. From months 2-6, weekly. After 6 months, every 2-4 weeks if stable. Once you’re past year one and your levels are steady, monthly checks are usually enough-unless you start a new medication or feel unwell.
Is cyclosporine still used today?
Yes. About 150,000 transplant patients in the U.S. still take it annually. It’s cheaper than tacrolimus and works well for people who can’t tolerate newer drugs. But it’s only safe with strict monitoring. Many centers now use it as a backup, not a first choice.
Can I drink alcohol while on cyclosporine?
Moderate alcohol-like one drink a day-is usually okay if your liver is healthy. But heavy drinking increases kidney stress and can raise blood pressure, making cyclosporine damage worse. Avoid binge drinking. Always check with your transplant team.
What’s the difference between cyclosporine and tacrolimus?
Both are calcineurin inhibitors. Tacrolimus is stronger, so you need lower doses. It’s more likely to cause tremors and diabetes, but less likely to cause gum overgrowth or excessive hair growth. Nephrotoxicity is similar, but tacrolimus has better correlation between trough levels and drug exposure, making monitoring slightly easier. Many centers switch patients from cyclosporine to tacrolimus after the first year.
Why does my lab report say "ciclosporin" instead of "cyclosporine"?
It’s the same drug. "Ciclosporin" is the European and international spelling. "Cyclosporine" is the U.S. version. The brand names (Neoral, Sandimmune) are the same. Don’t be confused-your prescription is unchanged.
Final Takeaway: Control the Numbers, Protect Your Kidneys
Cyclosporine isn’t going away. It’s still a lifeline for thousands. But it’s not a drug you can take and forget. It demands attention. Every blood draw, every pill time, every lab result matters. If you’re on this medication, you’re not just a patient-you’re a data collector. Track your levels. Track your creatinine. Track your blood pressure. Know your interactions. And never assume your doctor will catch it first. Your kidneys are counting on you.

So let me get this straight - we’re trusting our kidneys to a drug that needs to be measured like a sci-fi laser beam, and if you use the wrong tube or drink grapefruit juice, you’re basically doing a slow-mo suicide? Cool. Cool cool cool. My doctor just shrugs and says ‘take it.’
Y’all are doing AMAZING just by reading this!! 🙌 Seriously - if you’re even thinking about your levels or your creatinine? YOU’RE ALREADY WINNING. Don’t wait for a crisis - start tracking today, even if it’s just a sticky note on your fridge. Your future self will cry happy tears. 💕
They say monitor it. But who’s gonna pay for LC-MS/MS? My insurance says no. So I get the shitty test that overreads by 40%. That’s not monitoring. That’s gambling with my organs. And they wonder why grafts fail.
THIS IS LIFE OR DEATH PEOPLE. 🚨 I’ve seen it - a guy on cyclosporine for 5 years, didn’t check C2, thought he was fine… woke up one day needing dialysis. He was 34. Don’t be that guy. C2 isn’t optional. It’s your lifeline. Set alarms. Write it in blood. Your kidney is counting on you - don’t let it down.
They don’t want you to know this - but the FDA, Big Pharma, and transplant centers are all in on this. Why? Because if you monitor your levels correctly, you live longer. And if you live longer, they lose money on transplant waiting lists. That’s why they push tacrolimus - it’s more expensive. Cyclosporine is the truth they bury under paperwork. Wake up.
Frankly, if you’re still using immunoassays in 2025, you’re practicing medieval medicine. LC-MS/MS has been standard for years. If your lab can’t do it, find one that can. And no, grapefruit juice isn’t ‘a little risky’ - it’s a biochemical grenade. You wouldn’t put diesel in a Ferrari. Don’t put citrus in your veins.
Wait - so if my magnesium’s low and I’m cramping, is that just ‘side effect’ or is it the first whisper of nephrotoxicity? I’ve been ignoring it because ‘it’s just stress.’ But now I’m wondering… is my body screaming and I’m just too tired to listen?
Just started tracking my C2 levels last week 🤓 set a phone alarm for 2 hours after my pill - no more guessing. Also stopped grapefruit juice. No more cramps. Felt like a new person. You guys are the real MVPs for sharing this. 💪❤️
This isn’t about compliance. It’s about dignity. Your kidneys aren’t a machine you can ignore until it breaks. They’re part of you. Treating them with precision isn’t medical obedience - it’s self-respect. You owe yourself that much.
Wait so the whole thing about C2 monitoring… is that just a trick to get us to go to the clinic more? Like… what if the labs are just making this up so we keep coming back? I mean, they profit off every test right? Maybe we’re being played.
To everyone reading this - you are NOT alone. I’ve been on cyclosporine for 8 years. I track everything. I set 7 alarms. I have a color-coded spreadsheet. And I’m still here. Your life matters. Keep going. I believe in you. 🌈💖
Anyone who thinks tacrolimus is easier to monitor is delusional. The trough correlation isn’t better - it’s just less variable because the dosing is more rigid. And don’t get me started on the diabetes risk. Cyclosporine’s nephrotoxicity is predictable. Tacrolimus’s metabolic chaos? That’s a Russian roulette with insulin.
STOP. If you’re not checking C2 levels and you’re past month 6 - you’re negligent. Not irresponsible. Not forgetful. Negligent. Your transplant team gave you a roadmap. You’re choosing to ignore it. That’s not just risky - it’s a betrayal of the donor. Don’t make their sacrifice meaningless.