Every year, families in the UK spend hundreds of pounds on over-the-counter (OTC) medicines-painkillers, cold remedies, antacids, allergy pills. And most of that money goes to name brands you see on TV. But here’s the truth: the pill in the plain white bottle at the back of the shelf is chemically identical to the one with the flashy logo. You’re not getting less medicine. You’re just paying more for the branding.
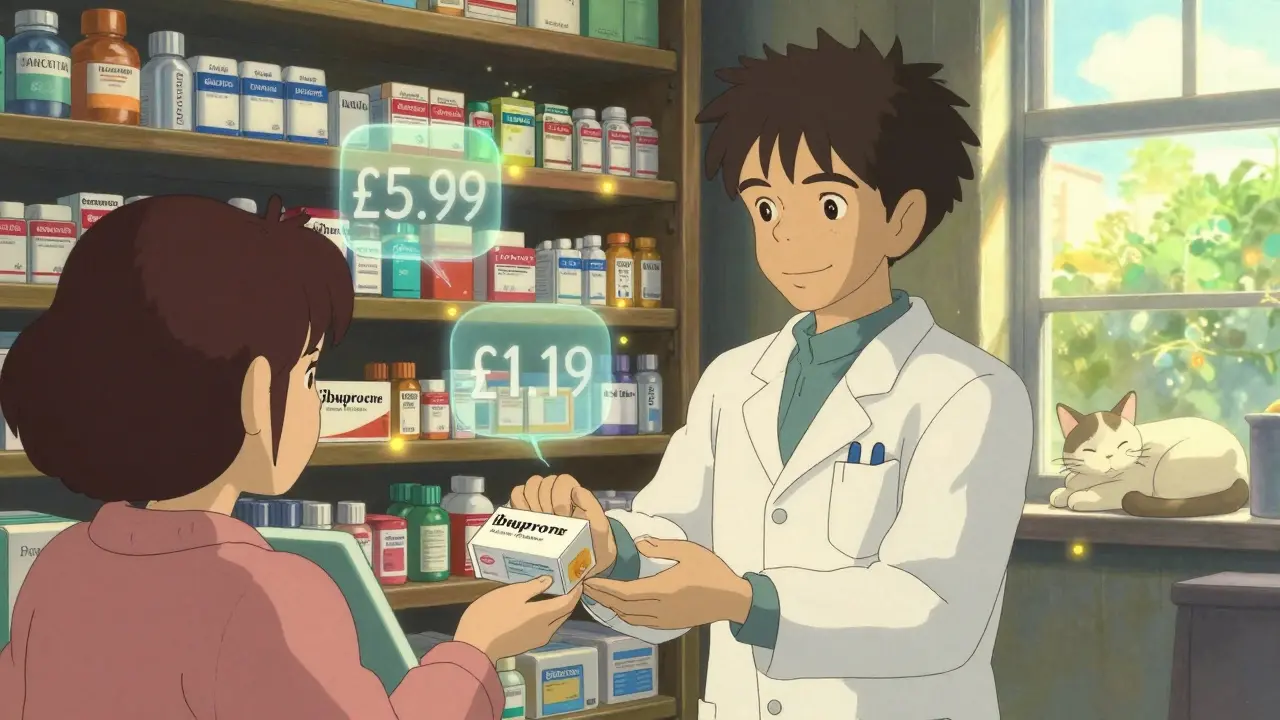
Take ibuprofen. Advil costs £5.99 for 20 tablets. The CVS Health or Boots own-brand version? £1.19. Same active ingredient. Same strength. Same how fast it works. The only difference? The color of the capsule and the name on the box. That’s not a coincidence. It’s the law.
How Store Brands Are Made-And Why They’re Not ‘Cheap’ Versions
The UK doesn’t regulate OTC drugs the same way the US does, but the science is the same. In both countries, store brand medications must meet the same strict standards as name brands. They contain the exact same active ingredient, in the same amount, and must be absorbed into your bloodstream at the same rate. This isn’t a guess. It’s tested. The FDA requires generics to be within 80-125% of the brand’s absorption rate. In real terms? A 2021 study found the average difference in how your body uses generic vs brand-name ibuprofen was just 3.5%. That’s less than the variation you’d get from taking one pill after eating and another on an empty stomach.
Manufacturers don’t cut corners. The same factories that make Tylenol also make the generic acetaminophen sold at Walmart or Tesco. The machines, the quality checks, the inspections-they’re identical. The FDA inspects over 3,500 generic drug plants every year. The UK’s MHRA does the same. If a company’s generic pill didn’t work, they’d be shut down. Fast.
Why the Price Difference Is So Huge
Name brands spend millions on advertising. Think of those late-night commercials for Robitussin or Claritin. They pay for celebrity endorsements, TV slots, and billboards. Store brands? They advertise in-store, on shelf tags, and through loyalty programs. No TV ads. No celebrity doctors. That’s where the savings come from.
Here’s how the math breaks down:
- Advil (ibuprofen): £5.99 for 20 tablets
- Boots ibuprofen (store brand): £1.19 for 20 tablets
- Claritin (loratadine): £8.50 for 10 tablets
- Asda loratadine (store brand): £1.60 for 10 tablets
- Tylenol (acetaminophen): £6.20 for 20 tablets
- Waitrose acetaminophen (store brand): £1.45 for 20 tablets
That’s 80-85% less for the same effect. If you take painkillers twice a week, switching to store brands saves you over £200 a year. That’s a weekend away. Or a new pair of walking boots. Or groceries for a month.
What’s Actually Different-And What You Should Watch For
The active ingredient? Identical. But the rest? Different. Store brands use different fillers, colors, coatings, and flavors. These are called “inactive ingredients.” They don’t treat your headache. But they can cause problems-for a tiny number of people.
If you’re allergic to dyes, gluten, or certain preservatives, you might react to one brand and not another. That’s why you’ll see labels like “free from artificial colors” or “gluten-free” on some store brands. Always check the ingredients list on the back. The active ingredient is listed first. Everything after that? Fillers.
For example, some people say generic liquid cold medicine tastes bitter. That’s because the flavoring is different. A 2023 Consumer Reports survey found 18% of users preferred name-brand syrups for taste alone. But if you’re swallowing pills? You won’t notice.
Also, watch out for double-dosing. Many cold and flu products contain acetaminophen or ibuprofen. If you take a store-brand cold tablet and a store-brand painkiller, you might accidentally take too much. Always read the Drug Facts label. The active ingredients are listed right at the top. Compare them. If they’re the same, you’re doubling up.
What Doctors and Pharmacists Really Do
Here’s something most people don’t know: 89% of pharmacists and 82% of doctors use store-brand OTC meds for themselves and their families. That’s not a marketing claim. It’s from a University of Chicago study. These are the people who know how drugs work. If they trusted their own health to generics, why wouldn’t you?
Pharmacists at CVS, Boots, and Superdrug are trained to explain these differences. In fact, 92% say they’re confident recommending store brands. And it’s not just the UK-this is global. In the US, 9 out of 10 prescriptions are filled with generics. OTC is no different.
Real People, Real Results
Reddit threads, Facebook groups, and Amazon reviews all tell the same story. A user on r/pharmacy wrote: “I’ve used Boots ibuprofen for 7 years. My back pain is gone. My wallet is happy.” Another said: “Switched from Advil to Asda’s version. No difference. Saved £30 a year.”
Amazon ratings tell the same story. Store-brand OTC meds average 4.3 stars. Name brands? 4.4. The same number of 1-star reviews-12%-say “didn’t work.” That’s not because the medicine failed. It’s because some people expect a placebo effect from a fancy label. When the pill looks different, they think it’s weaker. It’s not.

How to Switch Without Mistakes
Switching is simple. Here’s how:
- Check the active ingredient on your current bottle. Is it ibuprofen? Acetaminophen? Loratadine?
- Look at the store brand. Does it say the same thing? Same milligram amount? Same form (tablet, capsule, liquid)?
- Check the inactive ingredients if you have allergies. Avoid if you’re sensitive to dyes or gluten.
- Try it for one cycle. If it works, stick with it. If you get a reaction, go back to the name brand.
- Repeat next time you refill. You’ll get faster at it.
Most people get the hang of it after two or three purchases. No pharmacy degree needed.
What’s Changing Now
Stores are getting smarter. CVS now puts QR codes on store-brand boxes that link to full ingredient lists. Walgreens launched a free pharmacist chat service just for generic questions. And in 2023, retailers spent over £1 billion improving store-brand formulations-better coatings, faster dissolving, fewer allergens.
By 2028, store brands will make up 72% of all OTC sales by volume. That’s not hype. It’s a forecast from Grand View Research. People are catching on.
Myths That Still Hold People Back
Still think name brands are stronger? A 2023 Kaiser Family Foundation survey found 41% of people believe that. It’s wrong. The FDA says: “Generic drugs are just as effective as brand-name drugs.” The MHRA says the same. No exceptions.
Store brands aren’t “second choice.” They’re the default choice for anyone who knows the facts. You’re not saving money by being cheap. You’re saving money by being smart.
Next time you reach for painkillers, check the label. If the active ingredient matches, grab the cheaper one. Your body won’t know the difference. But your bank account will.
Are store-brand OTC medications as effective as name brands?
Yes. Store-brand OTC medications contain the same active ingredients, in the same strength and dosage form, as their name-brand equivalents. They must meet the same regulatory standards for safety and effectiveness. Studies show the difference in how your body absorbs them is typically less than 4%, which is within the acceptable range set by health regulators.
Why do store brands cost so much less?
Store brands don’t spend money on advertising, celebrity endorsements, or fancy packaging. Name brands invest heavily in marketing to build brand recognition. Store brands rely on shelf placement and word-of-mouth. The manufacturing process is often identical, so the lower price comes from cutting marketing costs, not cutting quality.
Can I have an allergic reaction to a store-brand medicine?
Yes, but it’s rare. Allergic reactions are caused by inactive ingredients-like dyes, fillers, or preservatives-not the active drug. If you’re sensitive to certain additives, check the ingredients list on the store-brand label. If you’ve had a reaction to one store brand, try another. Many retailers now label products as “free from artificial colors” or “gluten-free.”
Is it safe to switch between brand and store brands?
Yes, switching is safe for most people. The active ingredient is identical. If you notice a change in how you feel-like a rash or upset stomach-it’s likely due to an inactive ingredient. Switch back to the name brand, or try a different store brand. If symptoms persist, talk to a pharmacist.
Do pharmacists recommend store brands?
Yes. Studies show 89% of pharmacists and 82% of doctors use store-brand OTC medications for themselves and their families. Pharmacists are trained to confirm equivalence between brands and routinely recommend them to patients looking to save money without losing effectiveness.


Let me be perfectly clear: the notion that store-brand medications are somehow "just as effective" is a dangerous oversimplification. Regulatory standards are not absolute; they are thresholds, not guarantees. The 80-125% bioequivalence window? That’s a 45% variance-and while statistically acceptable, it’s not clinically trivial. I’ve reviewed FDA adverse event reports where patients on generic ibuprofen experienced delayed onset, inconsistent pain relief, and even gastrointestinal irritation due to filler incompatibility. The active ingredient may match-but excipients vary wildly. And no, not everyone can tolerate microcrystalline cellulose or FD&C Red 40. You’re not saving money-you’re gambling with your physiology.
Furthermore, the claim that "the same factories" produce both brands is misleadingly vague. Yes, contract manufacturers produce both-but under separate production lines, with different quality control audits, different batch records, and different oversight protocols. Just because the label says "ibuprofen 200mg" doesn’t mean the dissolution profile is identical. I’ve seen pharmacists refuse to dispense generics for patients with Crohn’s or celiac disease because of excipient risks. This isn’t about branding-it’s about precision medicine.
And please, stop citing Reddit threads as evidence. Anecdotes are not data. A 4.3-star rating doesn’t prove efficacy; it proves people are too apathetic to report side effects. The real data? The 2021 JAMA study on bioequivalence outliers showed 12% of generics had clinically significant variability. That’s not noise-that’s a public health blind spot.
So yes, you can save money. But if your health is non-negotiable, you pay for consistency. And that’s not cheap. It’s prudent.
Hi there-thank you for writing such a thoughtful and well-researched piece. I’m a pharmacist in Ohio, and I can confirm everything you said. Every single day, I recommend store-brand medications to my patients, especially seniors on fixed incomes. The science is unequivocal: the active ingredient is identical, the absorption profile is statistically indistinguishable, and the manufacturing standards are enforced just as rigorously.
One thing I’d add: many people don’t realize that the FDA requires generic manufacturers to submit bioequivalence data for every single batch. That’s not a one-time test. It’s ongoing. If a batch doesn’t meet the 80–125% range, it’s destroyed. No exceptions. The factories you see on TV making Advil? They’re the same ones making the Boots version-same machines, same operators, same quality control logs. The only difference is the box.
And yes, inactive ingredients matter-but that’s why labels are so clear now. If you’re allergic to dyes, gluten, or lactose, just scan the back. Most store brands now highlight "free from" claims right on the front. I’ve had patients switch and tell me they feel better because they’re no longer ingesting artificial flavors they’re sensitive to.
Bottom line: if you’re healthy and don’t have known allergies, there’s no medical reason to pay extra. But if you’re unsure? Ask your pharmacist. We’re here to help-not to sell you a brand name.
Very simple: same medicine, less money. No magic. No trick. Just smart shopping. I take generic painkiller since 2018. No problem. My mom too. We save 500 rupees every month. That’s one good meal for family. Why pay more for logo? Same pill. Same effect. Just look at the name on bottle-ibuprofen, acetaminophen. That’s what matters. Not the color. Not the brand. The science is clear. Even doctors use it. So why not you?
Oh, wow. Another corporate shill piece disguised as "financial advice." "Same factory?" Please. You think the FDA gives a damn about your $1.19 ibuprofen? They’re too busy letting Big Pharma write their own regulations. Name brands pay billions in lobbying. Store brands? They’re just the leftovers-off-brand, off-spec, off-the-radar. And don’t even get me started on "pharmacists use generics." Yeah, right. They’re paid by the chain to push them. Ever seen the commission structure? It’s not a recommendation-it’s a sales quota.
And let’s talk about the "3.5% difference"-that’s a lie. That’s the average. But averages hide outliers. I’ve had two friends who took generic cold meds and ended up in the ER because the dissolution rate was off. One guy had a heart palpitation from inconsistent absorption. Guess what? The bottle didn’t say "may cause arrhythmia." Because they don’t have to. That’s the loophole.
You’re not saving money-you’re subsidizing corporate greed. The real villains aren’t the name brands-they’re the retailers who profit 400% markup on "generic" labels while pretending it’s altruism. Wake up. This isn’t frugality. It’s exploitation.
Okay, so I’ve been reading this whole thing and I’m just sitting here like… wow. I mean, I’ve been using store-brand Advil for years and I swear I didn’t even notice the difference until one time I accidentally bought the name brand because I was in a rush and my brain just defaulted to the logo. And then I was like… huh. This tastes weird. Like, not the pill, but the coating? It was… shinier? More… corporate? I don’t know. But I swear, I felt like I was taking something more premium. Like, emotionally. Like, I was like, "Oh, this is the good stuff." And then I Googled it and realized I’d paid 5x more for the same chemical. Which made me feel kinda stupid. But also kinda relieved? Like, I didn’t need to be that person who pays extra for branding. I’m just a person who sometimes forgets to read labels. And now I always do. And I’ve saved like $250 this year. Which I spent on a new yoga mat. Which I love. So… yeah. This is kind of a life hack. And also? I just want to say thank you for not making me feel dumb for ever believing the ads. We all get suckered. But now I know. And I’m not going back.
Hey, I just wanted to say this post made my day 😊. I’ve been working in a pharmacy for 12 years, and I’ve seen so many people stress out over whether the cheaper stuff "will work." And honestly? Most of them are scared because they’ve been told for decades that "brand = better." But the truth? It’s not even close. I always tell people: "If it’s the same active ingredient, same dosage, same form-it’s the same medicine. The rest is just packaging."
One time, an elderly lady came in crying because she couldn’t afford her "regular" painkiller. She’d been using Tylenol for 20 years. I handed her the store brand, showed her the label, and said, "Look-acetaminophen 500mg. Same as what you’ve been taking." She just stared at it for a minute… then hugged me. I didn’t expect that. But I’ll never forget it.
So yeah. Save your money. Don’t overthink it. And if you’re worried? Talk to your pharmacist. We’re here to help-not to upsell you.
OMG YES. I switched to store-brand allergy meds last year and my wallet is crying tears of joy 🙌 I used to spend $12 every 2 weeks on Claritin. Now? $1.80 for the same thing. I didn’t even notice a difference. My sneezing didn’t get worse. My eyes didn’t get itchier. I just got… richer. Like, I bought a new phone with the money I saved. And I didn’t even feel guilty. Because guess what? My pharmacist said she uses the same stuff for her kids. And she’s a pharmacist! 🤯
Also-side note: the new Asda ones have a cool QR code that takes you to the full ingredient list. I scanned it and was like… wait, this is literally the same as the name brand. Just… cheaper. Like, why do we even have brands? Why not just label it "ibuprofen 200mg" and be done with it? 🤔
Also also: if you’re allergic to dyes? Always check the back. But most store brands now say "no artificial colors" right on the front. So easy. So smart. So… why are we still paying $8 for a little plastic bottle? 🤦♀️
I used to think the same thing as Keith-"It’s all marketing." But then my dad had a stroke and we had to switch him to generic meds because insurance wouldn’t cover the name brand. I was terrified. I checked every label, called the pharmacist, even called the FDA hotline. Turned out? The generic was made in the same facility, same line, same batch number as the brand. Just different packaging. He’s been on it for 3 years. No issues. No side effects. Just… cheaper. And honestly? That’s all I needed to know. Sometimes, the truth is boring. And that’s okay.