Narrow Therapeutic Index Drugs: What You Need to Know About Safe Use and Monitoring
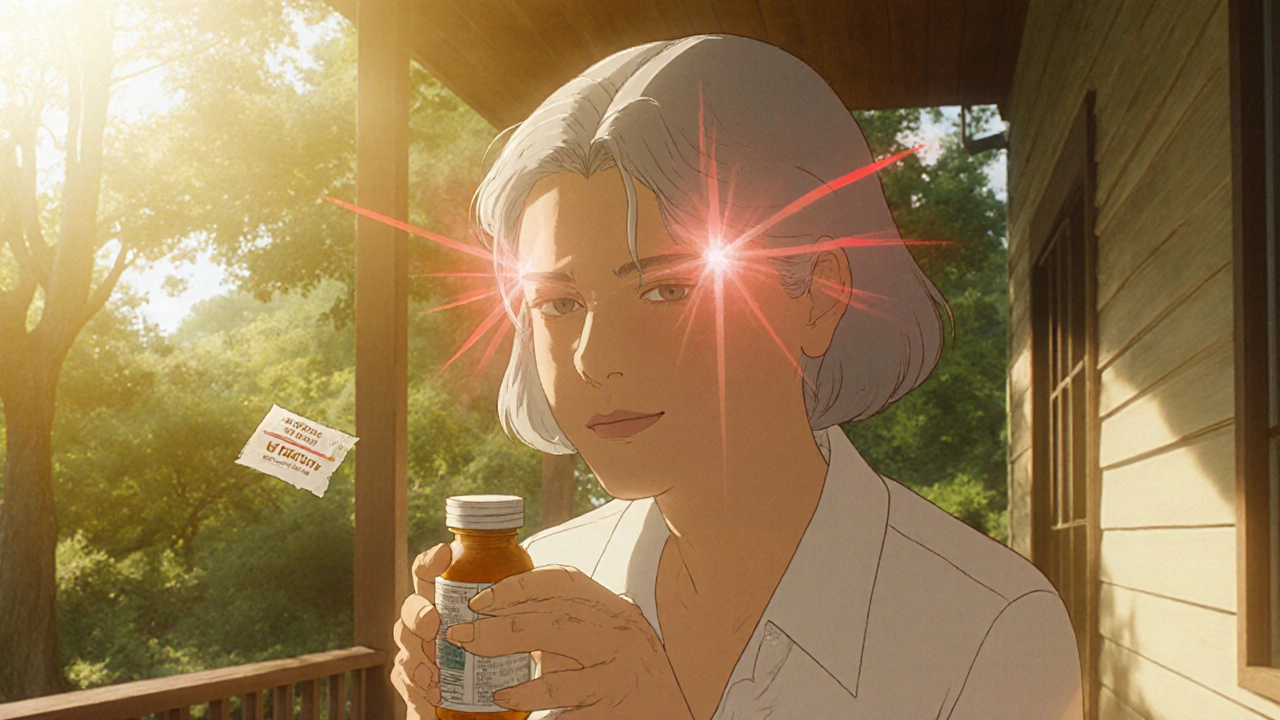
When a medication has a narrow therapeutic index, a small difference between the effective dose and the toxic dose. Also known as narrow therapeutic window drugs, these medications require extreme precision—too little won’t work, too much can kill you. Think of it like walking a tightrope: one misstep and things go wrong fast. Drugs like warfarin, digoxin, lithium, phenytoin, and cyclosporine fall into this category. They’re not rare—millions take them daily for conditions like heart failure, epilepsy, autoimmune disorders, and blood clots. But because their safety margin is so thin, even small changes in how your body processes them can lead to serious harm.
Why does this happen? Your liver, kidneys, age, other meds, or even what you eat can shift how much of the drug stays in your system. A single missed blood test or a new antibiotic can turn a safe dose into a dangerous one. That’s why therapeutic drug monitoring, regular blood tests to measure drug levels in your body isn’t optional—it’s life-saving. Pharmacists and doctors use these results to adjust doses in real time. And it’s not just about the pill you swallow—it’s about how your body handles it. That’s why medication adherence, taking your drug exactly as prescribed matters more with these drugs than almost any other. Skip a dose? Take an extra one? That’s not a mistake—it’s a risk.
These drugs also show up in stories you’ve probably heard: someone on warfarin bleeding after eating too much kale, or a patient with epilepsy seizing because their phenytoin level dropped after switching brands. That’s why generic versions aren’t always interchangeable here. Even tiny differences in how a generic is made can push levels out of the safe zone. That’s why your pharmacist might flag a switch—even if the label says "same active ingredient." And that’s why you need to talk to your provider before changing anything: diet, supplements, or even over-the-counter painkillers. Many of the posts below dive into real-world examples of these risks—like how aspirin affects blood thinners, or how antibiotics interfere with seizure meds. You’ll find guides on how pharmacists help patients avoid these traps, how to track your meds, and what to ask your doctor when you’re on one of these high-risk drugs.
There’s no sugarcoating it: narrow therapeutic index drugs demand respect. But they’re not something to fear—they’re something to manage wisely. With the right monitoring, communication, and awareness, you can use them safely. The posts here give you the tools to do exactly that—no jargon, no fluff, just clear, practical info you can use today.