Generic vs Brand Name Medications: What You Really Need to Know
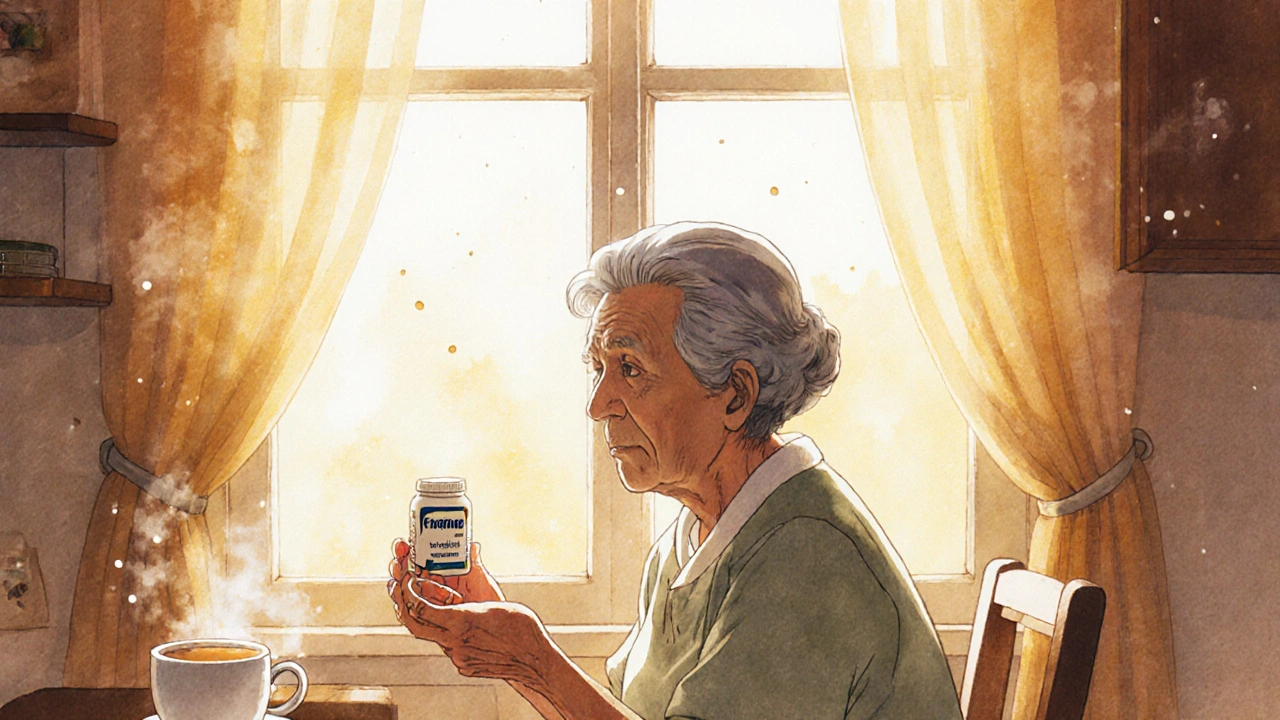
When you pick up a prescription, you might see two options: the familiar brand name or a cheaper generic version. Generic medication, a drug that contains the same active ingredient as a brand-name version, approved by the FDA to work the same way in the body. Also known as non-brand drugs, they’re not knockoffs—they’re legally required to match the brand in strength, dosage, and how fast they work. But here’s the thing: while they’re supposed to be identical, some people notice differences. That’s not just in their head. For drugs with a narrow therapeutic index, medications where even tiny changes in dose can cause serious side effects or reduced effectiveness—like warfarin, thyroid meds, or seizure drugs—switching between brands and generics can sometimes trigger symptoms. It’s not about quality. It’s about how the body reacts to small variations in inactive ingredients or how the pill breaks down.
That’s why brand name drugs, originally developed by pharmaceutical companies with patents and extensive clinical testing often feel more predictable. They’ve been on the market longer, and doctors and patients have more experience with them. But generics aren’t second-rate. Most of the time, they work just as well. The big difference? Cost. A generic version of a popular blood pressure pill can cost 80% less than the brand. That’s thousands saved a year. And the FDA doesn’t let companies cut corners—generics must prove they deliver the same amount of medicine into your bloodstream as the brand. Still, if you switch and feel off—new fatigue, dizziness, mood changes, or worse—don’t ignore it. Call your doctor. That’s not paranoia. That’s being smart.
Some people stick with brand names because their insurance pushes them to. Others switch to save money and never look back. There’s no one-size-fits-all answer. What matters is paying attention to how your body responds. If you’re on a critical medication, ask your pharmacist if the generic you’re getting is the same as the last batch. Keep a simple log: note when you switch, what you feel, and when. You’ll spot patterns faster than you think. The posts below cover real cases—from people who had seizures after switching generics to others who saved hundreds without a single issue. You’ll also find guides on how to spot when a generic might not be right for you, what to tell your doctor, and how to navigate insurance rules that force switches. This isn’t about fear. It’s about control. Your health, your rules.