Cyclosporine Nephrotoxicity: What You Need to Know About Kidney Damage from This Immunosuppressant
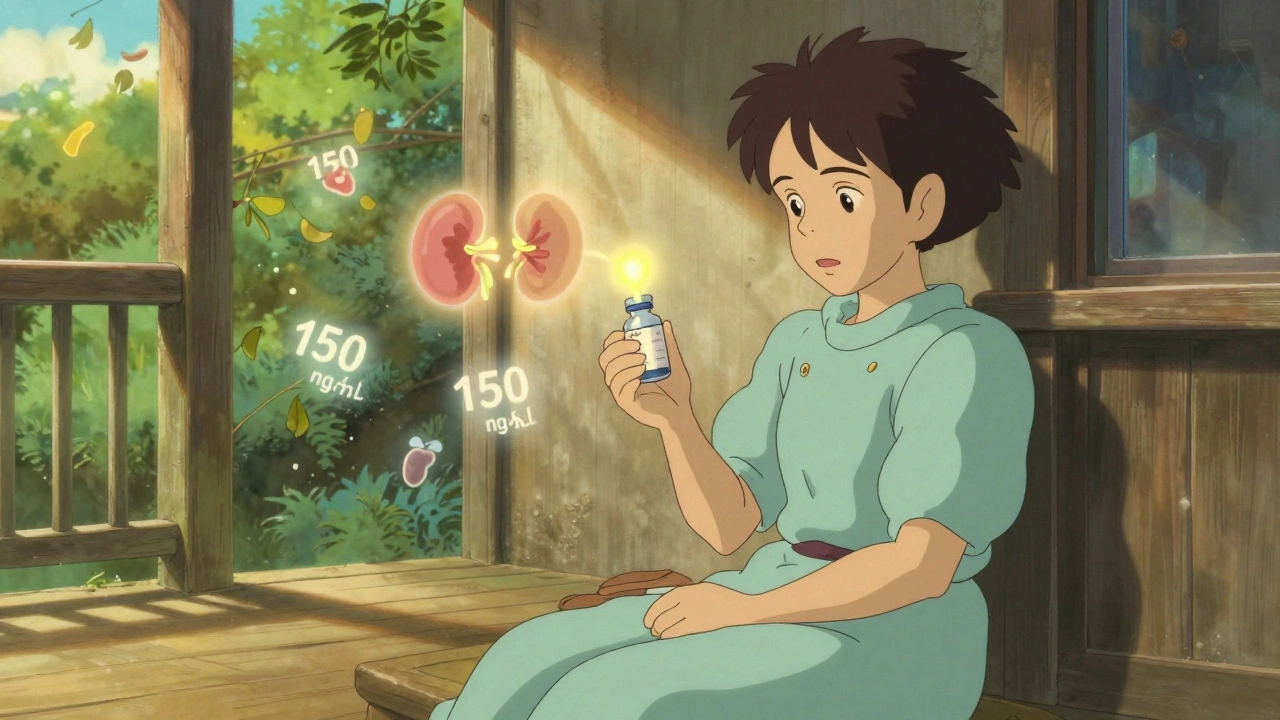
When you take cyclosporine, a powerful immunosuppressant used after organ transplants or for autoimmune conditions like psoriasis and rheumatoid arthritis. Also known as CsA, it stops your immune system from attacking your new organ or your own body—but it doesn’t stop from damaging your kidneys. This side effect, called cyclosporine nephrotoxicity, a type of kidney injury directly caused by the drug, is one of the most common reasons doctors have to adjust or stop treatment.
Cyclosporine narrows the tiny blood vessels inside the kidneys, reducing blood flow and filtering ability. Over time, this leads to rising creatinine levels, high blood pressure, and sometimes permanent scarring. It’s not rare—up to 50% of long-term users show some sign of kidney stress. The risk goes up if you’re older, have pre-existing kidney issues, take other kidney-toxic drugs like NSAIDs or certain antibiotics, or if your cyclosporine blood levels are too high. Many people don’t feel symptoms until the damage is advanced, which is why regular blood tests are non-negotiable.
There’s no magic fix, but you can lower your risk. Your doctor can monitor your kidney function with simple blood and urine tests. Switching to a different immunosuppressant like tacrolimus might help, though it comes with its own side effects. Staying well-hydrated, avoiding NSAIDs, and controlling your blood pressure are simple but powerful steps. Some patients benefit from switching to a once-daily formulation or using extended-release versions to smooth out drug levels. The goal isn’t to avoid cyclosporine entirely—it’s often lifesaving—but to use it smartly.
What you’ll find below are real-world insights from people who’ve dealt with this issue. From how to spot early warning signs to what alternatives exist, these posts give you the facts you need to talk to your doctor and protect your kidneys while staying on the treatment you need.