Imagine lying in bed, completely still, but your legs feel like they’re crawling with ants, buzzing with electricity, or aching as if you ran a marathon without ever standing up. You can’t sleep. You can’t relax. You just have to move. This isn’t a bad dream-it’s restless legs syndrome (RLS), a neurological condition that traps thousands in a nightly cycle of discomfort and exhaustion. And while dopamine-based drugs can offer quick relief, they often come with hidden costs that change lives in ways most people never expect.
What Really Happens in Your Brain With RLS?
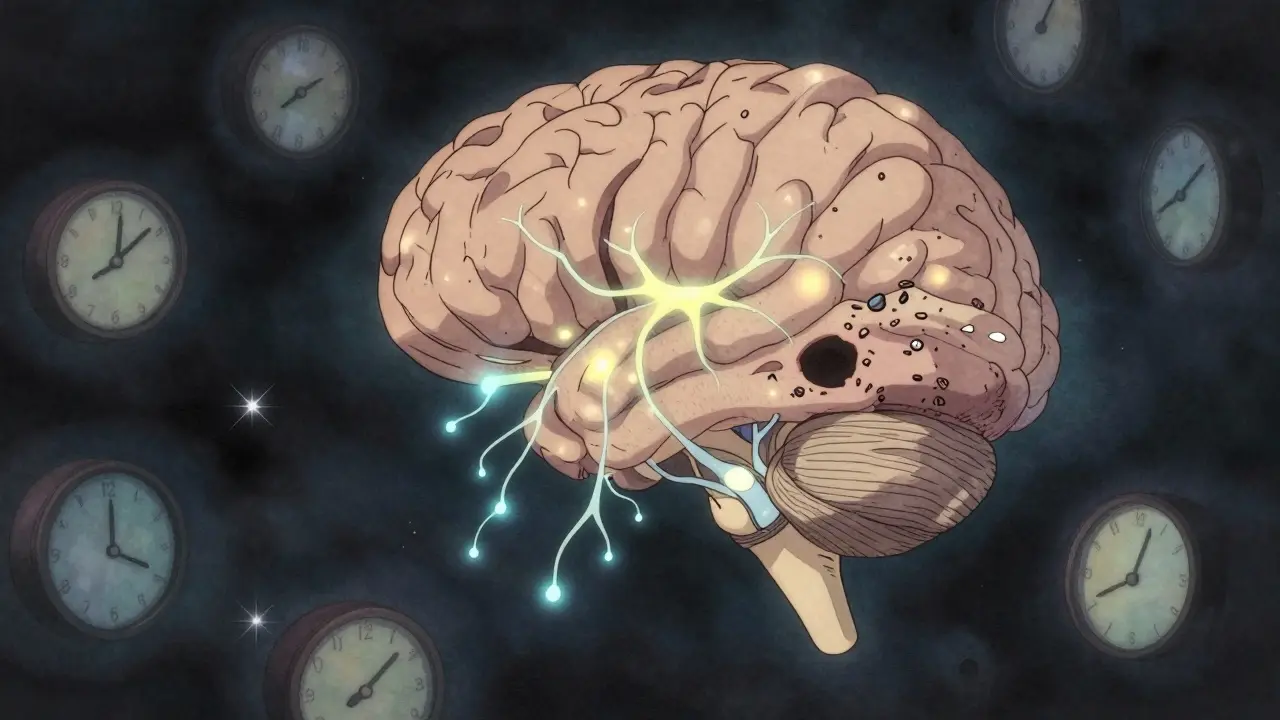
Restless legs syndrome isn’t just about twitchy legs. It’s a brain wiring problem. The urge to move comes from a glitch in the dopamine system-the same system that controls movement, reward, and sleep. In people with RLS, the A11 neurons in the brainstem, which send dopamine signals down to the spinal cord, don’t work right. Brain scans show these patients have 20-30% fewer dopamine transporters in the striatum compared to people without RLS. That means dopamine doesn’t get where it needs to go, and the result? Uncomfortable, restless legs that scream for movement.This isn’t random. RLS has a strong circadian rhythm. Symptoms spike between 8 p.m. and midnight-up to 400% worse than during the day. That’s why most people don’t notice it until they’re trying to fall asleep. And when they do lie down, the brain doesn’t switch into rest mode. Instead, it keeps firing signals that say: Move. Move. Move.
Iron deficiency plays a big part too. Many RLS patients have low iron in the substantia nigra, a brain region that produces dopamine. Even if blood tests look normal, the brain may still be starved. That’s why checking ferritin levels (not just iron) is critical. If your ferritin is under 75 ng/mL, iron therapy can cut symptoms by 30-40%-but it takes months to work.
How RLS Steals Your Sleep
Restless legs syndrome doesn’t just keep you awake. It ruins the quality of every minute you spend in bed. Polysomnography studies show people with RLS lose 30-50% of their total sleep time. They spend more time in light sleep (N1 and N2) and far less in deep, restorative slow-wave sleep. On average, they take 45-60 minutes to fall asleep-twice as long as someone without RLS. And once asleep? They wake up 6-10 times a night, often without even realizing it.And it’s not just the legs. About 80-90% of RLS patients also have periodic limb movement disorder (PLMD). That means their legs jerk every 20-40 seconds during sleep-sometimes 15 to 100 times an hour. These movements aren’t voluntary. They’re automatic, brain-driven spasms that fragment sleep even when the person doesn’t feel the urge to move.
The fallout is real. Daytime sleepiness scores average 12-14 on the Epworth scale (normal is 5-7). Working memory and attention drop by 20-30%. A 2022 meta-analysis found RLS patients are 2.3 times more likely to be in a car accident. For many, it’s not just fatigue-it’s a slow erosion of focus, safety, and mental clarity.
Dopaminergic Therapy: Fast Relief, Long-Term Risk
When symptoms are severe, doctors turn to dopamine agonists. These drugs-ropinirole, pramipexole, and rotigotine-mimic dopamine in the brain. They work fast. Most people feel relief within 1-2 hours. For someone who’s spent years unable to sleep, it’s life-changing.Here’s what the numbers say:
- Ropinirole (0.25-4 mg nightly): 47% symptom reduction in 12 weeks vs. 19% with placebo
- Pramipexole (0.125-0.5 mg): 40-50% improvement in IRLS scores
- Rotigotine patch (1-3 mg/24h): 45% reduction, with lower augmentation risk
But here’s the catch: these drugs don’t fix the problem. They mask it. And over time, the brain adapts. That’s when augmentation kicks in.
Augmentation means the symptoms get worse-not better. The urge to move starts earlier in the day. It spreads from legs to arms. The intensity climbs. What used to happen only at night now begins at noon. And the dose that once helped now feels like nothing.
Studies show 20-70% of patients develop augmentation within a year. Pramipexole has the highest risk-66% after three years. Rotigotine is better, at 26%. But even then, it’s not safe forever. The FDA requires a black box warning on all dopamine agonists because of this.
The Hidden Cost: Impulse Control Disorders
Beyond sleep, dopamine agonists can hijack your brain’s reward system. About 6-17% of users develop impulse control disorders. Gambling, compulsive shopping, binge eating, hypersexuality-these aren’t personality flaws. They’re drug side effects.One patient on Drugs.com wrote: “I spent $20,000 on online shopping I didn’t need. I didn’t even remember buying half of it.” Another on Reddit said: “I started visiting casinos every weekend. My wife found out when she saw my credit card statement.”
Men are more likely to develop gambling issues. Women report more shopping and eating disorders. The risk is higher if you have a history of depression, anxiety, or addiction. Yet most patients aren’t warned about this until it’s too late.
What Works Better in the Long Run?
There’s a better path for chronic RLS. Alpha-2-delta ligands-gabapentin enacarbil and pregabalin-don’t touch dopamine. Instead, they calm overactive nerves. They take 2-4 weeks to kick in, but they don’t cause augmentation. In a 2021 head-to-head trial, pregabalin (300 mg nightly) matched pramipexole in symptom relief but had only 8% augmentation vs. 32%.And iron? If your ferritin is low, IV ferric carboxymaltose can cut symptoms by 30-40%. It’s not quick. It takes months. But for those who respond, it’s a game-changer. No pills. No addiction risk. Just a simple infusion.
Non-drug strategies matter too:
- Avoid caffeine and alcohol after noon
- Walk or stretch for 10 minutes before bed
- Keep a consistent sleep schedule-even on weekends
- Try compression socks or warm baths
One patient on Reddit said: “I stopped drinking coffee at 2 p.m. and started walking my dog after dinner. I cut my pill dose in half. My legs still move, but now I sleep.”
How to Use Dopamine Drugs Safely
If you’re on a dopamine agonist, here’s how to protect yourself:- Start low. Ropinirole: 0.25 mg. Pramipexole: 0.125 mg. Never jump to the max dose.
- Take it 1-3 hours before symptoms usually start-not right before bed.
- Track symptoms weekly. Note: When do they start? How intense? Do they spread?
- Get ferritin tested every 6 months. If under 75 ng/mL, ask about iron therapy.
- Watch for signs of augmentation: symptoms starting earlier, spreading to arms, getting worse despite higher doses.
- Report mood changes, gambling urges, or uncontrolled spending to your doctor immediately.
Studies show 83% of augmentation cases are caught within 3 months if patients keep a symptom diary. Mayo Clinic reports 40% better outcomes when patients understand what to watch for.

The Future of RLS Treatment
New options are coming. In 2023, an extended-release version of ropinirole (Requip XL) was approved. It delivers steady levels of the drug, cutting augmentation risk from 31% to 18% in 12 months. Fipamezole, a new alpha-2 blocker, showed 35% less augmentation than pramipexole in early trials. Intranasal apomorphine is being tested for rapid, short-term relief without long-term exposure.Genetics may soon guide treatment. Variants in the BTBD9 and MEIS1 genes predict who’s more likely to respond to pramipexole-or who’s at high risk for augmentation. One 2022 study got 72% accuracy predicting outcomes based on DNA.
But here’s the hard truth: dopamine agonists still have a place. For severe, disabling RLS, they’re often the only thing that works. The goal isn’t to avoid them completely-it’s to use them wisely. Short-term. Low-dose. With monitoring. And always, always with a backup plan.
What Patients Really Say
A review of 1,247 patient experiences from Healthgrades, Drugs.com, and Reddit shows a clear divide:- 38% say dopamine drugs saved their lives: “Finally slept through the night after 15 years.”
- 62% say the cost was too high: “Augmentation turned my life upside down.”
- 78% of negative reviews mention symptoms worsening over time.
- 12% report impulse control problems.
- 65% of long-term users eventually switch to pregabalin or gabapentin.
There’s no one-size-fits-all. But the pattern is clear: dopamine works fast. But it doesn’t last. And the longer you use it, the more likely it is to break you.
Can restless legs syndrome go away on its own?
For most people, no. RLS is a chronic condition. In rare cases, it can be triggered by pregnancy, iron deficiency, or kidney disease-and may improve when the trigger is resolved. But for 70% of patients, especially those with a family history, it’s lifelong. That doesn’t mean it’s untreatable. It means you need a long-term plan, not just quick fixes.
Is there a cure for restless legs syndrome?
There’s no cure yet. But there are effective ways to manage it. Iron therapy can eliminate symptoms in people with low ferritin. Alpha-2-delta ligands like pregabalin offer long-term control without augmentation. Lifestyle changes help reduce severity. The goal isn’t to be symptom-free forever-it’s to find a balance that lets you sleep, function, and live without fear of the next night.
Why do dopamine drugs stop working over time?
Dopamine agonists don’t fix the brain’s dopamine shortage-they flood it with artificial signals. Over time, the brain responds by reducing its own dopamine receptors and transporters. This is called downregulation. The result? The drug becomes less effective, and symptoms return worse than before. That’s augmentation. It’s not tolerance-it’s the brain fighting back.
Can I take iron supplements instead of medication?
Only if your ferritin is low-below 75 ng/mL. Oral iron supplements often don’t work well because absorption is poor. IV ferric carboxymaltose is more effective and is recommended for RLS patients with confirmed iron deficiency. But if your ferritin is normal, taking extra iron won’t help and could even be harmful. Always get tested before starting.
What’s the safest long-term treatment for RLS?
For chronic, daily RLS, alpha-2-delta ligands like gabapentin enacarbil or pregabalin are now the first-line recommendation. They’re effective, don’t cause augmentation, and have fewer serious side effects than dopamine agonists. For intermittent symptoms, low-dose dopamine drugs are still appropriate-but only for short bursts. Iron therapy should always be considered if levels are low. Lifestyle changes are the foundation for everyone.
How do I know if I’m experiencing augmentation?
Look for three signs: 1) Symptoms start earlier in the day (e.g., now at 3 p.m. instead of 10 p.m.), 2) They spread to other body parts (arms, torso), and 3) They become more intense or require higher doses for the same relief. If you notice any of these, talk to your doctor. Don’t wait. Early detection can prevent full-blown augmentation.
Next Steps: What to Do Today
If you have RLS:- Get your ferritin level checked-don’t assume your iron is fine.
- Start a symptom diary. Track when symptoms start, how bad they are, and what helps.
- If you’re on a dopamine agonist, ask your doctor about augmentation risk and whether you’re on the lowest effective dose.
- Consider switching to pregabalin or gabapentin enacarbil if you’ve been on dopamine drugs for more than a year.
- Try non-drug strategies: evening walks, warm baths, no caffeine after 2 p.m.
RLS doesn’t have to control your life. But it demands respect. Quick fixes can backfire. Smart, sustained management works.


So let me get this straight-you’re telling me the same drugs that let me sleep for the first time in 15 years are slowly turning me into a compulsive online shopper with twitchy arms? Thanks, Big Pharma. At least my credit card has better taste than my brain does now.
The data presented is methodologically flawed. Augmentation rates vary wildly across studies due to inconsistent diagnostic criteria for symptom spread and temporal onset. Furthermore, ferritin thresholds of 75 ng/mL lack robust validation in neurologically symptomatic populations. The assertion that IV iron is 'more effective' ignores confounding variables such as baseline inflammation and hepcidin levels. This is not medicine-it’s anecdotal advocacy dressed in statistical clothing.
If you’re still on dopamine agonists after a year, you’re not managing RLS-you’re letting it manage you. Pregabalin isn’t just 'an option,' it’s the only responsible choice. Stop waiting for a miracle pill and start treating the root cause. Your brain isn’t broken-it’s just been betrayed by bad decisions. Time to wake up.
The paradox of dopamine therapy lies not in its pharmacology, but in its epistemology: we treat a deficiency by introducing an external mimic, thereby training the system to distrust its own signals. The brain, in its infinite wisdom, interprets this as an invasion-not a cure. Thus, augmentation is not a side effect, but a metaphysical rebellion. We seek equilibrium, yet offer chaos in the form of a pill. Perhaps the real illness is our refusal to accept that some rhythms cannot be hacked.
Neurotransmitter downregulation via chronic D2/D3 agonist exposure induces structural plasticity in the striatal medium spiny neurons, resulting in reduced dendritic arborization and altered GABAergic output. This is not tolerance-it’s neuroadaptive maladaptation. The FDA black box warning is underutilized in clinical practice due to cognitive bias toward symptom relief over longitudinal risk assessment. Ferritin thresholds remain arbitrary without cerebrospinal fluid biomarker correlation.
Of course you’re gonna get addicted to shopping if you’re on dopamine drugs. People like you think they can outsmart biology. You want a quick fix? Fine. But don’t cry when your life implodes because you thought your willpower was stronger than your neurochemistry.
For those of us in Southeast Asia, RLS is often dismissed as 'just stress.' I’ve seen grandmothers told to 'drink more milk' while their legs burned at night. This article is a lifeline. Thank you for naming what we’ve been told doesn’t exist. Iron infusions are still rare here-but now I know what to ask for.
Bro. I started gambling at 2am because my legs wouldn’t shut up. Lost $12k. My wife left. Now I’m on pregabalin. No more casinos. No more shame. Just sleep. And yeah, I still move-but now I don’t hate my body. You’re not weak. You’re wired wrong. Fix the wiring, not the guilt.
I used to think RLS was just 'bad sleep hygiene.' Then I started tracking my symptoms and realized: I wasn’t lazy-I was neurologically hijacked. Switching to pregabalin didn’t make me perfect, but it gave me back my nights. And honestly? The walking after dinner? That’s my new meditation. It’s not magic. It’s just… human. We’re not broken. We just need better tools.
Just wanted to say thank you for writing this. 🙏 I’ve been on ropinirole for 4 years and just found out I’m augmenting-symptoms started at 4pm now. I’m switching to pregabalin next week. You’re not alone. We got this. 💪
Let’s be real-dopamine drugs are like a Netflix binge: feels amazing in the moment, ruins your life by morning. I used to take pramipexole like candy. Now I walk my dog at dusk, skip coffee after 2, and take pregabalin. My legs still whisper. But they don’t scream anymore. You don’t need to be fixed-you need to be strategic.
For anyone reading this and feeling hopeless: you’re not failing. RLS is a beast, but it’s not unbeatable. Start with ferritin. Track your symptoms. Talk to your doctor about alternatives. Small steps. No shame. I’ve been there. You’re not broken-you’re just on the wrong path. Let’s find a better one together. 🤝
My dad had RLS. He took dopamine pills for 10 years. Then one day, he couldn’t sit still even during dinner. Arms, chest, even his jaw. We didn’t know it was the medicine. He just thought he was going crazy. This article? It’s the thing we needed 15 years ago.
The assertion that 'lifestyle changes are the foundation for everyone' is empirically unsupported. Controlled trials demonstrate that non-pharmacological interventions yield effect sizes of d < 0.3 for moderate-to-severe RLS. To prioritize behavioral modification over evidence-based pharmacotherapy is clinically irresponsible. This is not holistic medicine-it’s pseudoscientific reductionism.
Iron deficiency in the substantia nigra is real. But most doctors won’t test ferritin unless you beg. I had to go to a neurologist who specialized in movement disorders to get the test done. Took six months. Now I’m on IV iron. No pills. No gambling. Just sleep. If you’re reading this and still waiting for your doctor to take you seriously-keep pushing. You’re worth it.