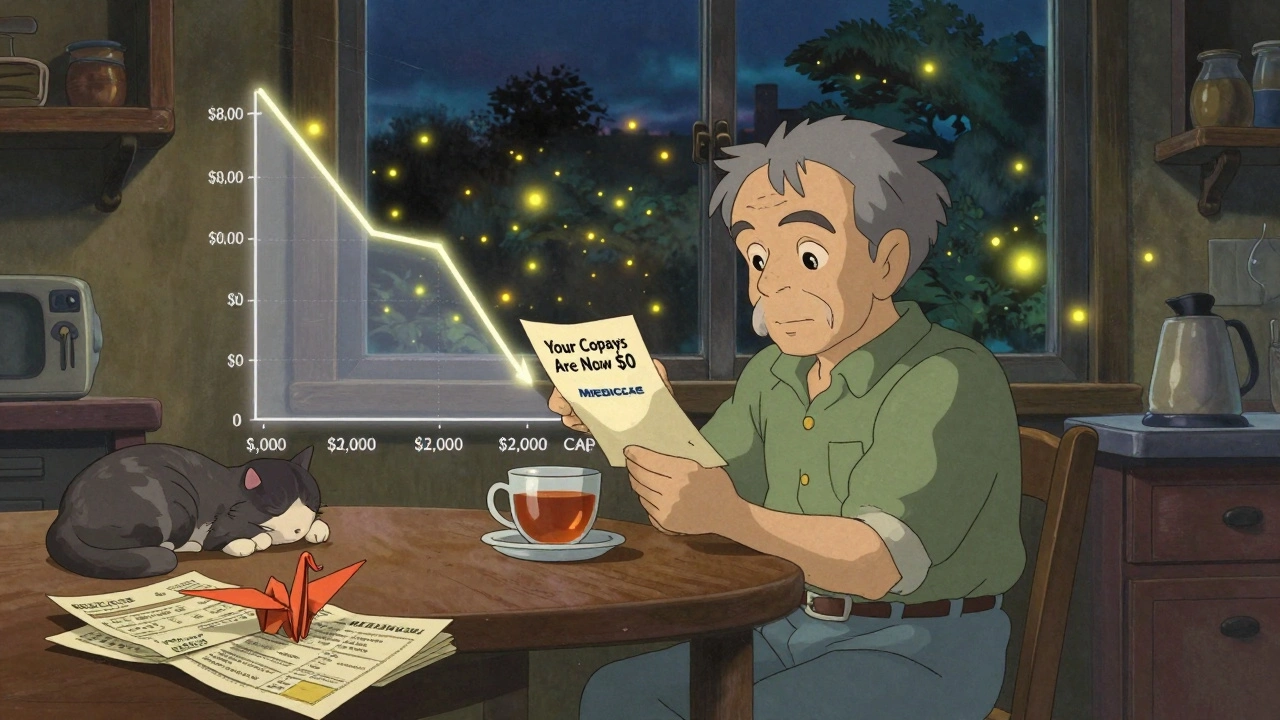
By 2025, Medicare Part D has changed the game for people who rely on generic medications. If you’re taking daily pills for high blood pressure, diabetes, or cholesterol, your out-of-pocket costs could drop by hundreds - even thousands - of dollars a year. The reason? A major overhaul of the program under the Inflation Reduction Act, which finally capped what you pay for prescriptions at $2,000 a year. That’s not a suggestion. It’s a hard limit. Once you hit it, your generic drugs cost you $0 for the rest of the year.
What Changed in 2025?
Before 2025, Medicare Part D beneficiaries could spend up to $8,000 out of pocket before reaching catastrophic coverage. Many seniors on multiple generic meds were stuck paying $100, $200, or more a month just to keep their medications. Now, thanks to the $2,000 out-of-pocket cap, that’s gone. You’ll pay the same amount for your generics whether you’re on your first pill or your 300th this year.The new structure is simple: After you pay your deductible (capped at $590 in 2025), you pay 25% coinsurance on generics until you hit $2,000. After that? Zero copays. No more surprises. No more choosing between meds and groceries.
How Much Do Generics Actually Cost Now?
For most people, the average copay for a 30-day supply of a preferred generic is around $10. That’s the same whether you’re on a stand-alone Part D plan or a Medicare Advantage plan with drug coverage. But here’s where it gets interesting: the monthly premiums are wildly different.On average, a stand-alone Part D plan costs $39 a month. A Medicare Advantage plan with drug coverage? Just $7. That’s a six-fold difference. So if you’re only taking generics, the cheaper plan isn’t just about lower copays - it’s about the whole package. Many people don’t realize they’re overpaying on premiums because they’re focused only on what they pay at the pharmacy.
And if you qualify for Extra Help (Low-Income Subsidy)? You’re looking at $0 deductible and $0 to $4.50 copays for generics. That’s not a discount. That’s a lifeline.
Why Some People Still Pay More Than They Should
The system isn’t perfect. Even with the new rules, 85% of Part D plans still have a deductible. That means if you’re on a plan with a $590 deductible and you take three generics that cost $40 each, you’ll pay the full price until you hit that cap. That’s $120 before you even get to the 25% coinsurance phase.Another problem: therapeutic substitution. Some plans swap one generic for another - not because it’s better, but because it’s cheaper for them. You might get your usual lisinopril one month, then get a different brand of lisinopril the next with a higher copay. You won’t know unless you check your explanation of benefits.
And then there’s the confusion around what counts toward your $2,000 cap. Monthly premiums? No. Manufacturer coupons? Yes - but only if they’re applied correctly. Some people think their $50 discount from the drugmaker doesn’t count, but it does. That’s called TrOOP - true out-of-pocket spending. If you don’t understand it, you might think you’re far from the cap when you’re actually halfway there.
Plan Differences: PDP vs. MA-PD
There are two main ways to get Part D coverage: a stand-alone Prescription Drug Plan (PDP) or a Medicare Advantage Prescription Drug plan (MA-PD). Both cover generics, but the trade-offs are real.PDPs are separate from your Medicare coverage. You pay a premium, and you use your Original Medicare for doctor visits. MA-PDs bundle everything - doctors, hospital care, and drugs - into one plan. They often have lower premiums, but you’re stuck with a network. If your doctor isn’t in-network, you pay more.
For someone taking only generics, MA-PDs usually win. Lower premiums, same copays, same $2,000 cap. But if you need specialist care or travel often, a PDP might give you more flexibility. The key is to compare not just copays, but total annual cost: premiums + out-of-pocket spending.
Who’s Saving the Most?
The biggest savings go to people who take multiple generics. Someone on five generic drugs, each costing $40 a month, would have paid $2,400 a year before 2025. Now, after hitting the $2,000 cap, they pay nothing for the rest of the year. That’s $1,200 saved - just from one year of the new rules.According to the Centers for Medicare & Medicaid Services, the average beneficiary taking generics will save about $400 a year. But for those on high-volume regimens, savings can top $1,000. That’s not theoretical. Reddit users like ‘RetiredPharmacist2023’ say they went from paying $1,200 more last year for the same meds to $0 this year.
Even more telling: 68% of Part D enrollees taking generics say they’re satisfied with their coverage - up from 59% in 2023. That’s a clear signal the changes are working.
What You Need to Do Right Now
Don’t wait until next year. Here’s what to do in the next 30 days:- Log into Medicare Plan Finder and enter your exact medications. Use the generic names - not brand names.
- Filter for plans with the lowest total cost: premium + estimated copays for your drugs.
- Check if your plan uses step therapy or prior authorization on your generics. If yes, call the plan and ask for a list of covered alternatives.
- See if you qualify for Extra Help. Even if you think your income is too high, you might still qualify. The income limit for 2025 is $21,597 for individuals.
- Call 1-800-MEDICARE if the Plan Finder is confusing. They can walk you through your options.

The Bigger Picture: Why Generics Matter
Generics make up 84% of all prescriptions filled under Part D - but only 27% of total drug spending. That’s the power of generics. They’re not just cheaper. They’re the reason Medicare Part D is still financially viable. Without them, the program would collapse under the weight of brand-name drug prices.The Inflation Reduction Act didn’t just help seniors. It forced drugmakers to cap price increases. If a generic’s price jumps more than inflation, the manufacturer has to pay a rebate to Medicare. That keeps costs down for everyone.
And it’s getting better. By 2028, generic use in Part D is expected to rise to 87%. New biosimilars - generic versions of complex biologic drugs - are starting to appear. These could bring savings similar to traditional generics, but for conditions like rheumatoid arthritis and cancer.
What’s Still Broken?
Despite the progress, problems remain. The reinsurance system has shifted. Now, insurance companies bear more of the cost after the $2,000 cap. Some are responding by restricting access to higher-cost generics - even if they’re medically necessary. You might find your plan suddenly requires you to try a cheaper generic first, even if your doctor says it won’t work for you.Also, 41% of beneficiaries still don’t understand how manufacturer discounts count toward the $2,000 cap. That’s why so many call Medicare’s helpline confused. They think they’re paying more than they are - or worse, they think they’re not making progress toward the cap.
The system works best when you know how it works. Don’t assume your plan is the best one. Don’t assume your copay won’t change. Check every year.
Final Thought: You’re Not Overpaying - You’re Just Uninformed
The truth is, most people on Medicare don’t realize how much they could save. They stick with the same plan year after year because it’s easier. But in 2025, the math has changed. Your generic meds might now cost you $0 after October. You just need to know where to look.Don’t wait for a bill to surprise you. Don’t assume your plan is fair. Take 20 minutes now. Use the Plan Finder. Compare your drugs. Call if you’re stuck. You’ve paid into this system your whole life. It’s time to get what you’re owed.
Do generic drugs cost less under Medicare Part D in 2025?
Yes. Thanks to the $2,000 out-of-pocket cap introduced in 2025, most people pay significantly less for generics. After hitting the cap, your copays drop to $0 for the rest of the year. Median copays for preferred generics are around $10 per 30-day supply before reaching the cap, and many plans now offer $0 deductibles for those who qualify for Extra Help.
What’s the difference between a PDP and an MA-PD for generic drug coverage?
Both cover generics the same way under the standard Part D structure - same $2,000 cap, same copays. But PDPs are standalone drug plans with higher premiums (around $39/month), while MA-PDs bundle drug coverage with Medicare Advantage and usually cost $7/month. MA-PDs often have lower total annual costs for people taking only generics, but you’re limited to their provider network. PDPs let you see any doctor who takes Medicare, but cost more overall.
Does the $2,000 cap include my monthly premium?
No. Only what you pay at the pharmacy counts toward the $2,000 out-of-pocket cap. That includes your deductible, copays, and coinsurance for generics and brand-name drugs. Monthly premiums, pharmacy fees, and non-covered drugs don’t count. This is a common misunderstanding - make sure you’re tracking only your actual drug payments.
Can my plan switch my generic medication without telling me?
Yes - and this is called therapeutic substitution. Your plan can replace one generic version of a drug with another, even if they’re chemically identical, if the new version is cheaper for them. They must notify you, but not always in time. Always check your formulary each year. If your copay suddenly jumps, it’s likely because your plan swapped your generic for a different one with a higher tier.
How do I know if I qualify for Extra Help?
You may qualify if your income is below $21,597 (single) or $29,169 (married) in 2025, and your resources are under $11,760 (single) or $23,520 (married). Extra Help gives you $0 deductible, $0-$4.50 copays for generics, and no coverage gap. Apply at SSA.gov or call 1-800-772-1213. Even if you think you don’t qualify, check - many people do without realizing it.
Why do some people still pay more than $2,000 for drugs?
You won’t pay more than $2,000 for covered drugs under Part D in 2025 - that’s the cap. But if you take non-covered drugs, get prescriptions filled outside your plan’s network, or use brand-name drugs without prior authorization, those costs won’t count toward the cap. Also, if you don’t enroll in a Part D plan and get charged a late penalty, you’ll pay more overall. The cap only applies to what’s covered by your plan.
Should I switch plans every year just for generics?
Yes - especially if you take multiple generics. Plans change their formularies, copays, and networks every year. What was the cheapest plan last year might be the most expensive this year. Use the Medicare Plan Finder every fall during Open Enrollment (October 15-December 7). Even small changes in copays can add up to hundreds in savings over a year.


Finally some real relief for seniors on meds
You people don't get it. This isn't charity. This is the government finally doing its job after decades of letting Big Pharma rob us blind. The $2,000 cap is the bare minimum and if you're still complaining about premiums you're part of the problem. We paid into this system our whole lives and now you're whining about $7/month? Get over it.
I switched to an MA-PD last year and my total yearly cost dropped from $1,800 to $412. I take five generics and now I pay $4.50 per script after October. I didn't even know manufacturer coupons counted toward the cap until I read this. So glad I finally checked my plan details. You guys really need to log into Medicare Plan Finder. It's not hard, I promise.
My copay went up last month for my metformin even though I'm on a generic and I didn't change plans. I called and they said they swapped it for a different generic that's in a higher tier. No warning. No notice. This is still a mess
YESSSSS THIS IS WHAT WE NEEDED 😭🙏 I went from paying $1,200 a year to $0 after October last year. My grandma cried when she saw her first $0 copay. This is life changing. Tell everyone you know to check their plan. Don't just roll over!
Anyone who thinks this is a win hasn't looked at the reinsurance burden shifting to insurers. The real cost is being passed on through restricted formularies and prior auth hoops. You think you're saving money but you're just being herded into cheaper alternatives your doctor didn't prescribe. This is regulatory capture disguised as reform
Man this is wild. In Nigeria we pay full price for generics and still can't get them sometimes. Here you guys got a cap and you're still arguing about $7 premiums? I'm glad you got this but don't forget how lucky you are
OMG I JUST REALIZED I WAS OVERPAYING FOR 3 YEARS 😱 I was on a PDP paying $39/month and my copays were $15 each. I switched to an MA-PD for $7 and now I'm at $0 after October. I almost missed this. I'm telling everyone on Facebook. This is the best thing that's happened to Medicare since 2006
Typo in the article: 'TrOOP' not 'Troop'... and no one's correcting it? Seriously? The whole point is understanding what counts toward the cap and you're all missing the basic term. How are people not getting this?
Don't let anyone tell you this isn't a win. I'm 72 and on three generics. Last year I was choosing between insulin and groceries. This year I'm not even thinking about it. The system still has flaws but this? This is dignity. You deserve to take your meds without fear. Keep checking your plan every year. You're worth it.
So now we're rewarding people who took out expensive brand name drugs before 2025? The cap rewards bad behavior. Why should I pay less because I took 3 different meds? The system should reward smart choices not reckless spending. This is just socialism with a nice label
Quick question: if you're on Extra Help and your plan has a $0 deductible, does the $2,000 cap still apply? Or do you just pay $0 all year regardless? I'm trying to figure out if I'm getting the full benefit
Let's be real - the real winners here are the insurers. They get to offload costs to Medicare after $2,000, and they still get to cherry-pick which generics to cover. They're not losing money. They're just playing the long game. You think you're getting a deal but you're just being nudged toward cheaper options that might not work as well. The system is still rigged.
Just switched to an MA-PD. My plan changed my generic from lisinopril to benazepril. My doctor says they're not equivalent for me. I called the plan and they said 'it's the same thing.' I'm going to file a grievance. This is how they get you. Don't trust them. Check your EOB every month.
Thanks for the tip about manufacturer coupons counting toward TrOOP. I just checked my last 3 months and realized I was already 40% of the way to the cap. I didn't even know. This changes everything.