FRID Medication Risk Checker
Check if your medications increase fall risk and get safer alternatives.
Enter a medication name above to check if it increases fall risk in seniors.
Note: This tool identifies medications that are classified as Fall Risk Increasing Drugs (FRIDs). Always consult your healthcare provider before making any medication changes.
Falls are the leading cause of injury-related death for adults over 65. Every year in the U.S., 36 million falls happen, leading to 3 million emergency room visits and 32,000 deaths. Many of these falls aren't accidents-they're side effects of sedating medications that cause dizziness, sleepiness, or balance problems.
Sedating Medications are drugs that slow down the central nervous system, often used for anxiety, sleep issues, or pain. While helpful for their intended purpose, they can cause dangerous side effects like dizziness, confusion, and unsteadiness that increase fall risk in older adults.Why Sedating Medications Increase Fall Risk
These medications affect your brain and body in ways that make falls more likely. Benzodiazepines for anxiety or sleep can leave you groggy and uncoordinated. Opioids for pain slow your reaction time. Even antidepressants might cause dizziness when you stand up. The problem gets worse when you take multiple sedating drugs at once-a situation called polypharmacy. It happens when older adults take three or more medications daily, and each extra drug raises fall risk significantly.
According to the CDC, seniors on just one sedating medication have a 20% higher fall risk. With two or more, that risk jumps to 50% or more. This isn't just about accidents-it can lead to broken hips, brain injuries, or even death. The good news? Many of these falls are preventable with the right strategies.
The STEADI-Rx Approach: A Three-Step Strategy
STEADI-Rx is a CDC initiative designed to help healthcare providers reduce medication-related fall risk. It uses a simple three-step process: screen for fall risk, assess modifiable factors, and intervene with evidence-based strategies.Here's how it works in practice:
- Screen: Use the CDC's fall risk assessment tool during routine checkups. Ask simple questions like "Have you fallen in the past year?" or "Do you feel unsteady when standing?"
- Assess: Review all medications for FRIDs (Fall Risk Increasing Drugs). This includes checking for drug interactions and whether the dose is too high.
- Intervene: Work with pharmacists and doctors to adjust medications, suggest non-drug alternatives, and recommend exercise programs.
This approach isn't just theoretical. A 2021 study showed STEADI-Rx could prevent over 42,000 medically treated falls and save $418 million in healthcare costs each year in the U.S. It's especially effective in community pharmacies where pharmacists take the lead on medication reviews.
Key Medications That Raise Fall Risk
| Medication Class | Common Examples | Primary Fall Risks | Safer Alternatives |
|---|---|---|---|
| Benzodiazepines | Diazepam, Lorazepam | Drowsiness, dizziness, impaired balance | Non-sedating sleep aids, CBT for insomnia |
| Opioids | Oxycodone, Hydrocodone | Dizziness, slow reaction time | Non-opioid pain relievers, physical therapy |
| Antidepressants | Sertraline, Duloxetine | Dizziness, especially when starting | Therapy, non-sedating antidepressants |
| Antipsychotics | Quetiapine, Risperidone | Sedation, confusion | Non-pharmacological approaches, lower doses |
One real-world example: A 78-year-old man on diazepam for anxiety had three nighttime falls in a month. His pharmacist reviewed his medications and suggested switching to cognitive behavioral therapy for insomnia (CBT-I) instead. Within six months, his falls stopped completely. This isn't uncommon-75% of STEADI-Rx recommendations involve switching to safer alternatives.
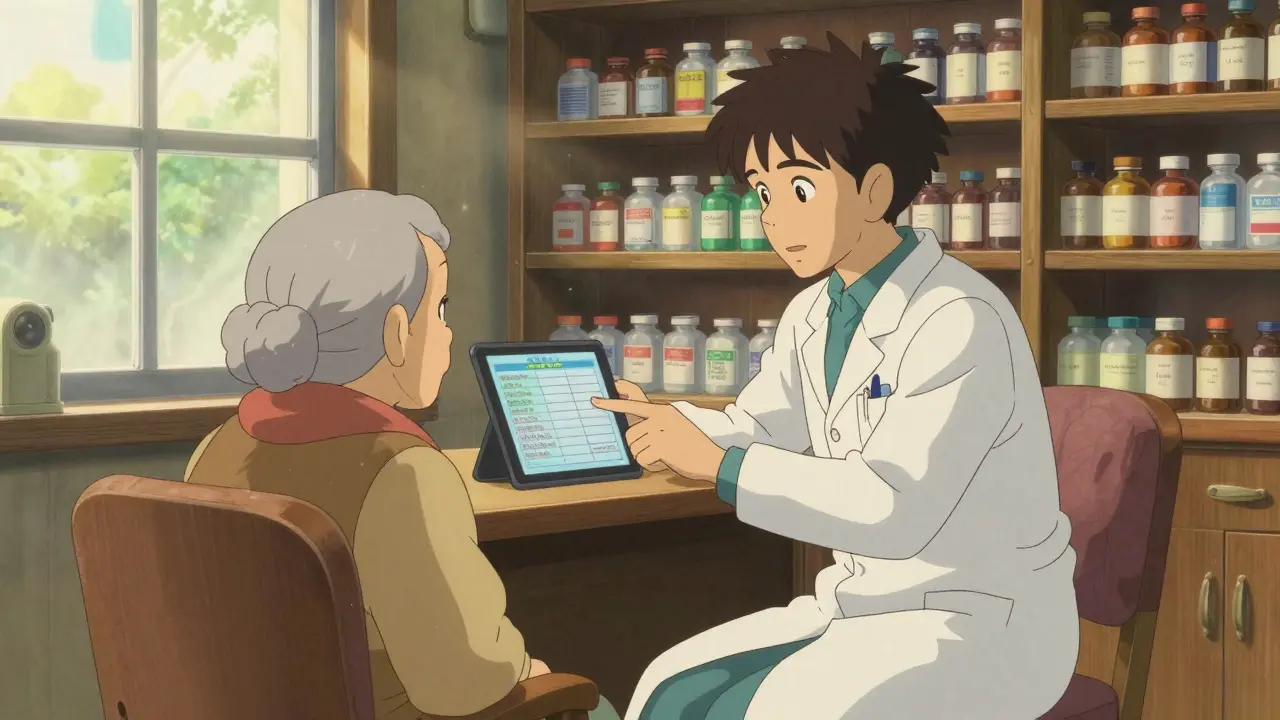
How Medication Reviews Prevent Falls
Pharmacists are your secret weapon for fall prevention. They don't just count pills-they check for hidden dangers. In the STEADI-Rx model, pharmacists document medication therapy problems and share findings with doctors using a Provider Consult Form. This form includes answers to three key questions:
- Is this medication necessary?
- Is the dose too high?
- Are there safer alternatives?
For example, a pharmacist might notice a patient taking both an opioid and a benzodiazepine. These drugs together multiply fall risk. The pharmacist could recommend switching the opioid to a non-opioid pain reliever like acetaminophen, or suggest physical therapy for chronic pain. This collaborative approach cuts fall risk by up to 30% compared to medication changes alone.
Many seniors don't realize pharmacists can help with this. In fact, a 2022 survey found only 45% of pharmacists feel they have enough time to do comprehensive reviews. But when they do, the results speak for themselves. A 2023 study in the Journal of the American Geriatrics Society showed medication reviews reduced falls by 22% in older adults.
Combining Medication Management with Other Strategies
Medication reviews alone aren't enough. The best results come from combining them with other simple changes:
- Exercise: Balance training, strength exercises, and walking programs reduce falls by 15-29%. Aim for 30 minutes, three times a week. Even simple moves like standing on one foot or heel-to-toe walking help.
- Home safety: Remove tripping hazards like loose rugs, install grab bars in the bathroom, and improve lighting. A 2021 study found these changes cut home falls by 35%.
- Vitamin D: While research is mixed, the U.S. Preventive Services Task Force recommends 800 IU daily for seniors. It's especially helpful for those with low vitamin D levels.
When these strategies work together, the impact is powerful. A 2020 Cochrane review found that combining medication reviews with exercise programs reduced fall-related fractures by 61% and medical care visits by 43%. This isn't just about avoiding falls-it's about staying independent longer.
Overcoming Common Challenges in Deprescribing
Changing medications isn't always easy. Many seniors worry about withdrawal symptoms or symptom return. A 2021 National Council on Aging survey found 63% of older adults struggle to reduce sedating medications due to these fears. Doctors may also hesitate, especially if they're short on time.
But solutions exist. Electronic health record alerts can flag high-risk medication combinations. Clear communication between pharmacists and doctors ensures safe transitions. Patient education materials explain risks and benefits in plain language. For example, explaining that "stopping this medication might feel scary at first, but it could keep you from falling" helps build trust.
One success story: A 72-year-old woman on multiple sedating drugs for anxiety and sleep had frequent falls. Her pharmacist created a gradual tapering plan with her doctor, replacing one medication at a time. After three months, she was on safer alternatives and had zero falls. This shows that with patience and teamwork, deprescribing works.
Should I stop taking my sedating medication on my own?
Never stop a medication without consulting your healthcare provider. Suddenly stopping can cause dangerous withdrawal symptoms. Work with your doctor and pharmacist to create a safe plan.
Which medications are most likely to cause falls?
Benzodiazepines (like Valium), opioids (like oxycodone), antidepressants (like Zoloft), and antipsychotics (like quetiapine) are top offenders. These drugs slow brain function and impair balance. Always ask your pharmacist to review all your medications for fall risks.
How can a pharmacist help with fall prevention?
Pharmacists review all your medications, check for interactions, and suggest safer alternatives. They also coordinate with your doctor to adjust prescriptions safely. In the STEADI-Rx model, pharmacists are key partners in reducing fall risk. Ask them to do a medication review during your next visit.
Is exercise really effective for preventing falls?
Yes. Programs focusing on balance, strength, and gait training reduce falls by 15-29%. Even simple exercises like standing on one foot or heel-to-toe walking can help. Aim for 30 minutes, three times a week. The CDC offers free exercise guides for seniors online.
What should I do if I've already fallen?
Report the fall to your doctor immediately. They'll assess your risk, review your medications, and recommend preventive steps. Don't ignore it-falling once doubles your chance of falling again. Keep track of when and where falls happen to help your doctor identify patterns.


My grandma's on diazepam and I just learned about the fall risks. Gotta share this with her doc. 🙌
That's great you're taking action! Many seniors don't realize how common this issue is. The STEADI-Rx program is a fantastic resource for doctors and pharmacists. It's amazing how simple changes like medication reviews can prevent falls. Keep spreading the word!
36 million falls occur each year in the U.S., many linked to sedating medications
The STEADI-Rx approach offers a clear three-step strategy for healthcare providers
However, implementation varies widely across different healthcare settings
Rural areas often lack access to pharmacists and specialists, exacerbating the problem
Many elderly patients are prescribed multiple sedating medications without thorough review, increasing fall risks significantly
It's crucial that healthcare systems invest in better coordination between doctors, pharmacists, and patients
Public awareness campaigns could help seniors understand the risks and encourage discussions about alternatives
The economic impact is staggering, with billions spent annually on emergency care and rehabilitation
Investing in prevention now could save substantial resources
Training programs for healthcare providers on STEADI-Rx protocols should be mandatory
Electronic health records should include alerts for high-risk medication combinations
Collaboration between government agencies and healthcare institutions is essential for a comprehensive strategy
Without systemic changes, fall-related injuries will continue to rise
We must act now to protect our most vulnerable population
Pharmacists play a vital role in reviewing medications and suggesting safer alternatives
Many seniors on sedating meds face fall risks daily Why isn't more being done to address this #fixthis
India faces similar issues 🌍 Many seniors here are on sedating meds without proper reviews We need global awareness 🙏 #healthcare
Healthcare systems need to prioritize fall prevention for seniors America should lead in implementing STEADI-Rx Let's get our healthcare system in check 🤝
America leads? Hardly Most seniors don't have access to proper care This article ignores systemic issues It's easy to blame meds but the real problem is lack of training for doctors
It is imperative that healthcare providers prioritize patient safety The STEADI-Rx guidelines are clear and must be implemented universally Failure to do so is not only negligent but also unethical