Combining blood thinners with common pain relievers like ibuprofen or naproxen isn’t just a bad idea-it’s a medical danger that puts you at risk of severe, even fatal, bleeding. This isn’t theoretical. It’s backed by hard data from a 2024 study of over 51,000 people in Denmark, and the numbers don’t lie. If you’re on a blood thinner and reach for an over-the-counter pain pill, you’re playing Russian roulette with your internal organs.
What Happens When Blood Thinners Meet NSAIDs
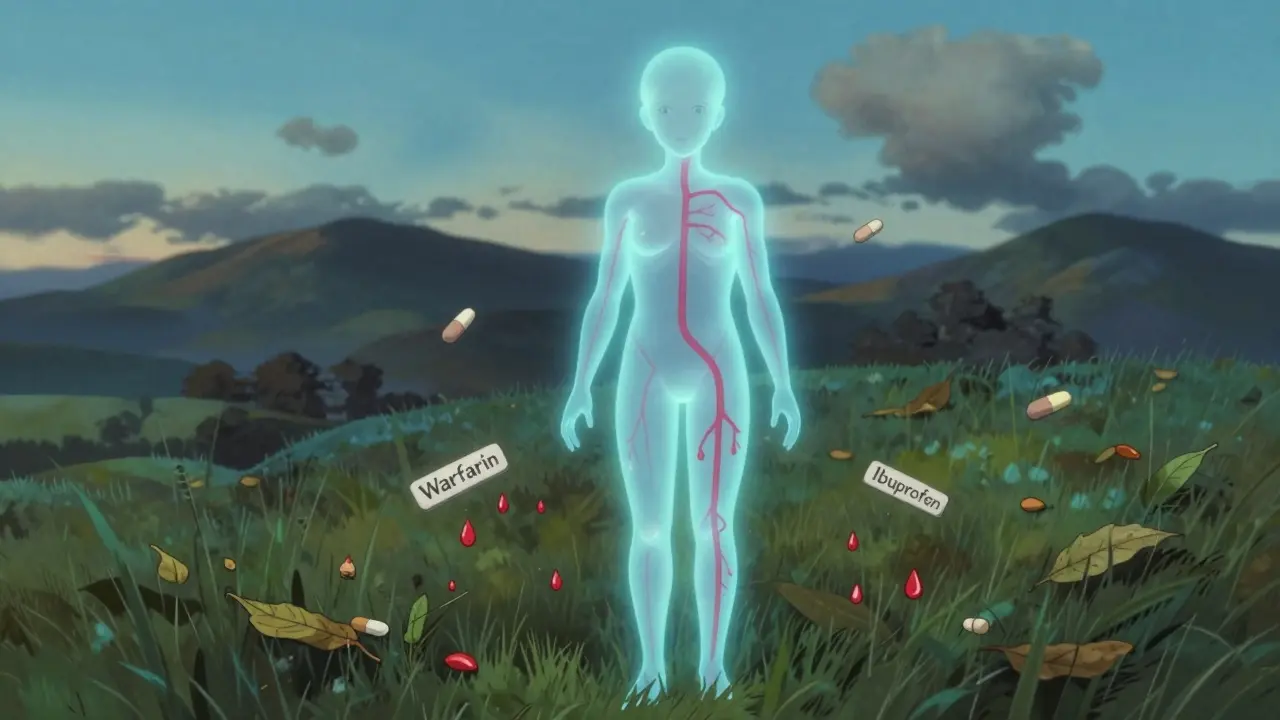
Blood thinners-whether they’re warfarin, apixaban, rivaroxaban, or dabigatran-work by slowing down your blood’s ability to clot. That’s necessary if you have atrial fibrillation, a history of clots, or a mechanical heart valve. But NSAIDs like ibuprofen, naproxen, and diclofenac do something different: they stop your platelets from sticking together. Platelets are the first responders when you cut yourself. Without them, bleeding doesn’t stop easily.Put them together, and you’ve got a one-two punch. Your blood can’t clot properly, and your platelets can’t do their job. The result? Bleeding that starts small and can spiral out of control. This isn’t just about stomach upset. The Danish study showed this combo doesn’t just raise your risk of gastrointestinal bleeding-it triples your chance of bleeding in your brain, lungs, and urinary tract.
The Numbers Don’t Lie: How Much Risk Are You Really Taking?
Not all NSAIDs are created equal when it comes to bleeding risk. The Danish study broke it down clearly:- Naproxen: 4.1 times higher risk of hospitalization for bleeding
- Diclofenac: 3.3 times higher risk
- Ibuprofen: 1.79 times higher risk
Even ibuprofen, which many people think is "safe" because it’s available over the counter, nearly doubles your bleeding risk. And here’s the kicker: it doesn’t matter if you’re on an older blood thinner like warfarin or a newer one like apixaban. The risk is the same across the board. There’s no "safer" blood thinner when NSAIDs are in the mix.
The study also found:
- 2.24 times higher risk of stomach and intestinal bleeding
- 3.22 times higher risk of bleeding in the brain
- 1.57 times higher risk of bleeding in the urinary tract
- Almost three times higher risk of severe anemia from internal bleeding
These aren’t rare events. In a population of 51,000 people, this combination sent hundreds to the hospital for emergency bleeding. And that’s just the ones who made it to the ER. Many more likely had minor bleeds that went unnoticed until they became serious.
Why Even "Low Dose" or "Short Term" Doesn’t Save You
You might think: "I only take ibuprofen once in a while for a headache." Or: "I’m on it for a week after my knee surgery. That’s not long enough to matter." That’s a dangerous assumption.The Danish study showed that even short-term use-just a few days-significantly increased bleeding risk. There’s no safe window. The moment you take an NSAID while on a blood thinner, your body’s ability to control bleeding is compromised. And because the damage is cumulative, repeated use-even spaced out over months-keeps your risk elevated.
Doctors often tell patients to take NSAIDs with food or add a stomach pill like omeprazole to protect the gut. But here’s the truth: those measures only help a little. They might reduce stomach ulcers, but they do nothing to stop bleeding in your brain, lungs, or kidneys. The risk isn’t just in your stomach-it’s everywhere.
What You Should Use Instead
If you’re on a blood thinner and need pain relief, you have options. The safest and most effective alternative is acetaminophen (Tylenol). It doesn’t affect platelets or clotting. It won’t raise your bleeding risk. It’s not a miracle drug-it doesn’t reduce inflammation like NSAIDs-but for pain like headaches, back pain, or arthritis discomfort, it works well for most people.For chronic joint pain, physical therapy, heat packs, or cold therapy can help reduce reliance on pills. Weight management, gentle movement, and braces or supports also reduce pain without drugs. If you have severe arthritis or gout, talk to your doctor about alternatives like colchicine or corticosteroid injections. These don’t interfere with blood thinners the way NSAIDs do.
And if you’re using NSAIDs for something like a sprained ankle or a bad toothache? Limit it to 2-3 days max. Even then, check with your doctor first. Don’t assume it’s okay just because it’s sold next to aspirin at the pharmacy.
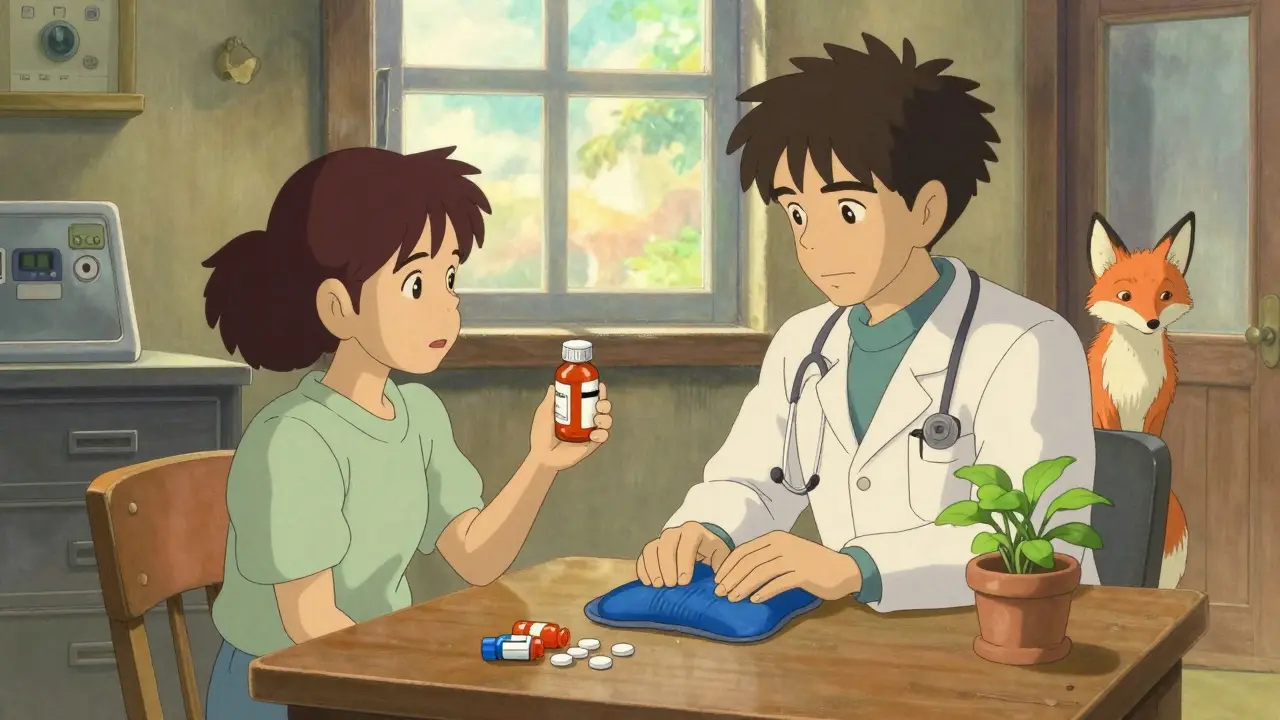
What Your Doctor Should Be Asking You
Most patients don’t think of ibuprofen or naproxen as "medications." They say, "I just take Advil now and then." But doctors need to ask directly: "Are you using any over-the-counter painkillers?" And they need to ask every time you visit.Studies show that nearly half of patients on blood thinners who take NSAIDs never mention it unless asked. That’s because they don’t see it as a drug interaction-they see it as a casual fix. But it’s not. It’s a medical risk.
Good doctors now use electronic alerts in their systems to flag patients on anticoagulants who are prescribed NSAIDs. But those alerts only work if the NSAID is prescribed. What about the ones bought at the pharmacy? That’s where you have to be your own advocate.
Keep a list of everything you take-prescription, over-the-counter, supplements, herbal teas. Bring it to every appointment. If your doctor doesn’t ask about NSAIDs, ask them: "Is it safe for me to take ibuprofen with my blood thinner?" If they say yes, ask why. Push for evidence. This isn’t a conversation you should leave to chance.
Why This Problem Is Getting Worse
More people than ever are on blood thinners. Atrial fibrillation, deep vein thrombosis, and stroke prevention mean millions are on these drugs. At the same time, NSAID use is skyrocketing. In the U.S. alone, over 30 billion OTC ibuprofen tablets are sold each year. That’s a lot of people combining two high-risk drugs without realizing it.Regulators have warnings on the labels, but they’re easy to miss. Pharmacies don’t always flag the interaction at checkout. And many patients assume, "If it’s sold over the counter, it must be safe." That’s exactly the myth that’s costing lives.
The American College of Cardiology now recommends that health systems actively identify patients on both types of drugs and help them switch to safer alternatives. That’s a start. But real change happens when patients stop treating NSAIDs like candy and start treating them like the powerful drugs they are.
What to Do Right Now
If you’re on a blood thinner:- Check your medicine cabinet. Do you have ibuprofen, naproxen, diclofenac, or aspirin? Put them away. Don’t just store them-get rid of them if you don’t have a clear, doctor-approved reason to keep them.
- Switch to acetaminophen for pain. Start with 500 mg every 6-8 hours as needed. Don’t exceed 3,000 mg per day unless your doctor says otherwise.
- Write down any pain you’re trying to manage. Is it joint pain? Headaches? Back pain? Bring this list to your next appointment and ask: "What’s the safest way to treat this without raising my bleeding risk?"
- If you’ve taken an NSAID in the last week, tell your doctor. Even if you think it was "just once."
This isn’t about fear. It’s about control. You’re already managing a serious condition. Don’t let a simple painkiller undo your progress. The right pain relief exists. You just have to choose it wisely.
Can I take aspirin with my blood thinner?
Aspirin is an NSAID and an antiplatelet drug, so combining it with a blood thinner significantly increases bleeding risk-just like ibuprofen or naproxen. Even low-dose aspirin (81 mg) used for heart protection should not be taken with anticoagulants unless your doctor specifically recommends it for a clear reason, like after a stent placement. Never start or stop aspirin on your own.
Is Tylenol (acetaminophen) really safe with blood thinners?
Yes, acetaminophen is the safest over-the-counter pain reliever for people on blood thinners. It doesn’t affect platelets or clotting factors. However, it’s not without risks-taking more than 3,000 mg per day can damage your liver, especially if you drink alcohol or have liver disease. Stick to the lowest dose that works and never exceed the daily limit.
What about topical NSAIDs like Voltaren gel?
Topical NSAIDs are absorbed through the skin, so they enter the bloodstream in much smaller amounts. Some studies suggest they carry a lower bleeding risk than pills, but they’re not risk-free. If you’re on a strong blood thinner, even topical NSAIDs could contribute to bleeding. Talk to your doctor before using them. For most people, a heating pad or ice pack is safer and just as effective for localized pain.
Can I take NSAIDs if I’ve been on blood thinners for years without problems?
Just because you haven’t bled yet doesn’t mean you’re safe. Bleeding events are unpredictable. The Danish study showed that risk increases immediately after taking an NSAID, regardless of how long you’ve been on a blood thinner. Many patients who ended up hospitalized had been on anticoagulants for years without incident-until they took ibuprofen for a sore knee. The longer you’re on a blood thinner, the more vulnerable you become to this interaction.
What should I do if I accidentally took an NSAID with my blood thinner?
If you took one dose of an NSAID and feel fine, monitor yourself for signs of bleeding: unusual bruising, dark or bloody stools, red or pink urine, severe headaches, dizziness, or weakness. Call your doctor immediately if any of these appear. Even if you feel okay, it’s still important to tell your doctor. They may want to check your blood levels or adjust your medication plan. Don’t wait for symptoms-this interaction can be silent until it’s too late.


Just had my mom go through this last year-she was on apixaban and took naproxen for her arthritis "just once" because her doctor didn’t warn her. Ended up in the ER with a GI bleed. She’s fine now, but I’ll never let anyone in my family touch NSAIDs again. Acetaminophen is your BFF here. Seriously, if you’re on a blood thinner, treat OTC painkillers like live grenades.
Also, if your doctor says "it’s fine," ask them to show you the study. Most don’t even know the Danish data. Don’t be polite-be alive.
so you're telling me i cant take advil for my hangover after drinking wine and eating tacos while on xarelto?? bro i just wanna feel human again
this is all a pharma scam. the real cause of bleeding is glyphosate in your food and the government forcing you to take blood thinners so they can track you. ibuprofen is natural, aspirin is from willow bark, and they're scared because you can buy it for $2. they want you dependent on $500/month pills. read the FDA’s 1998 leaked memo-search "warfarin NSAID coverup". I’ve got screenshots.
why you guys always focus on west medicine? in india we use turmeric paste and cold water compress for pain. no drugs needed. also why you take blood thinner at all? your diet is too much processed food. fix that first. then you dont need any pills
I’ve been on rivaroxaban for five years and never even considered ibuprofen a "drug." It’s just… what you take. The fact that this interaction is so poorly communicated is terrifying. I’m going to print this out and give it to my GP. I’ve had two friends end up in hospital from this exact combo. One was 68, healthy, just took a few naproxen for a bad back. Didn’t see it coming. No one warned them.
It’s not just medical negligence-it’s cultural. We treat OTC like candy. We need to change that.
Let’s be precise: acetaminophen is metabolized by the liver, and while it doesn’t affect coagulation, it can cause hepatotoxicity in supratherapeutic doses-especially in those with preexisting liver impairment or alcohol use. The 3,000 mg/day limit isn’t arbitrary; it’s evidence-based. Also, note that some extended-release formulations may have different safety profiles. Always check the active ingredient, not just the brand name. Tylenol, Panadol, Mapap-all contain acetaminophen. Excedrin? Contains aspirin. Read the label like your life depends on it-because it does.
And yes, topical diclofenac still has systemic absorption. One study showed plasma concentrations up to 12% of oral dosing. That’s enough to tip the scales in high-risk patients. Don’t assume topical = safe.
This is one of those silent killers that flies under the radar because people don’t think of Advil as medicine. I’ve worked in ERs for 12 years and seen this exact scenario too many times. A patient comes in with a headache, says they took two ibuprofen, and we find them with a massive intracranial bleed. They didn’t even realize it was dangerous.
My advice: keep a medication log. Write down everything-supplements, teas, OTCs. Bring it to every appointment. If your doctor doesn’t ask about NSAIDs, ask them. It’s not being difficult-it’s being smart. You’re not just managing a condition-you’re managing your survival.
Why do Americans always need pills for everything? In India, we use yoga, massage, and cold water. No drugs. Also, why are you so dependent on Western medicine? You think a pill fixes everything? Your body is weak because you eat junk and sit all day. Fix your lifestyle first. Then you won’t need blood thinners or painkillers. This whole post is just fear-mongering by Big Pharma to sell more Tylenol.
And why are you so scared of natural pain? Pain is your body’s warning. You should listen, not silence it with chemicals.
bro i took ibuprofen with warfarin for 3 years and still alive 😎 maybe it’s just luck? 🤷♂️ also i drink whiskey every night so i think i’m invincible 🍸💉
Oh my god. This is the most important thing I’ve read all year. I’ve been on apixaban since 2020 and I’ve been popping Advil like Skittles. I thought it was fine because I didn’t have stomach pain. I’m literally shaking right now. I just threw out my entire cabinet. I’m calling my doctor tomorrow. This isn’t just advice-it’s a life-saving intervention. Thank you for writing this. I feel like I almost died today without knowing it.
The ethical imperative here transcends pharmacology. It speaks to a broader failure in health literacy and the commodification of bodily autonomy. We have allowed pharmaceutical marketing to redefine "safety" as mere availability, when true safety requires contextual understanding, professional guidance, and personal responsibility.
It is not enough to issue warnings on labels. We must cultivate a culture where patients are empowered not merely to consume, but to interrogate, to inquire, and to resist the normalization of risk. This is not merely about bleeding-it is about the dignity of informed choice.
Just had a patient come in last week-72, on dabigatran, took diclofenac for a month after a fall. No symptoms until she passed out from internal bleeding. Turned out her hemoglobin was 5.8. She didn’t even realize she was bleeding internally. No black stools, no pain-just weakness. That’s the scary part. It’s silent.
And yeah, acetaminophen is the answer, but here’s the kicker: many elderly patients can’t tolerate it because of liver issues. So what then? Physical therapy, weight loss, braces, heat. Simple stuff. But no one wants to do the work. We want the pill. That’s the real problem.
i took ibuprofen with my blood thinner and nothing happened so its fine
As a physician in Delhi, I see this daily. Patients on anticoagulants come in with NSAID use because they trust the pharmacist more than their doctor. We need better community education. Also, many use Ayurvedic pain balms that contain camphor or wintergreen oil-both have salicylate-like effects. They think "natural" means safe. It doesn’t.
Always ask: what’s the active ingredient? Not the brand. Not the packaging. The chemical. That’s the only thing that matters.
I’ve been on warfarin for 10 years and I take ibuprofen every weekend for my golf back. My INR’s always fine. You’re all panicking over nothing. I’ve got more sense than you lot. Stop scaring people with science-y nonsense.