When you’re managing asthma, inhaled corticosteroids (ICS) are often the most effective tool you have. They calm inflammation in your airways, prevent flare-ups, and help you breathe easier day after day. But if you’ve been using them for months or years, you might have noticed a sore throat, a hoarse voice, or even unexplained bruising. These aren’t just random annoyances-they’re signs that the very medication keeping you healthy might be causing other problems. The good news? Most of these side effects are avoidable. You don’t have to choose between breathing well and feeling unwell. With the right technique, dose, and monitoring, you can keep your asthma under control without paying a heavy price.
What Are the Real Side Effects of Asthma Steroids?
Not all side effects are the same. Some are local-happening right where the medicine touches your body. Others are systemic, meaning they affect your whole body, even though the drug was meant to stay in your lungs. The most common local side effects include:
- Oral thrush: A white, patchy fungal infection in the mouth or throat. It’s not dangerous, but it’s uncomfortable and can make swallowing hard.
- Hoarseness or voice changes: Your voice might sound raspy or weaker than usual. This happens when the steroid irritates your vocal cords.
- Throat irritation or cough: A scratchy throat after using your inhaler is common, especially if you don’t rinse afterward.
Systemic side effects are rarer-but more serious. They usually show up only with long-term, high-dose use:
- Adrenal suppression: Your body’s natural stress hormone production slows down. You might feel tired, dizzy, or get sick more easily under stress.
- Skin thinning and easy bruising: Especially in older adults or people on high doses for over five years. A light bump might leave a mark that lasts weeks.
- Bone density loss: Long-term use above 750 mcg/day of beclomethasone equivalent increases fracture risk, especially in women over 65.
- Increased pneumonia risk: For people over 65, high-dose ICS raises the chance of lung infections. The risk jumps from about 5% to nearly 9% per year.
- Growth delay in children: At standard doses, kids might grow 0.7 cm slower per year-but this doesn’t affect their final adult height. High doses (above 800 mcg/day) carry more risk.
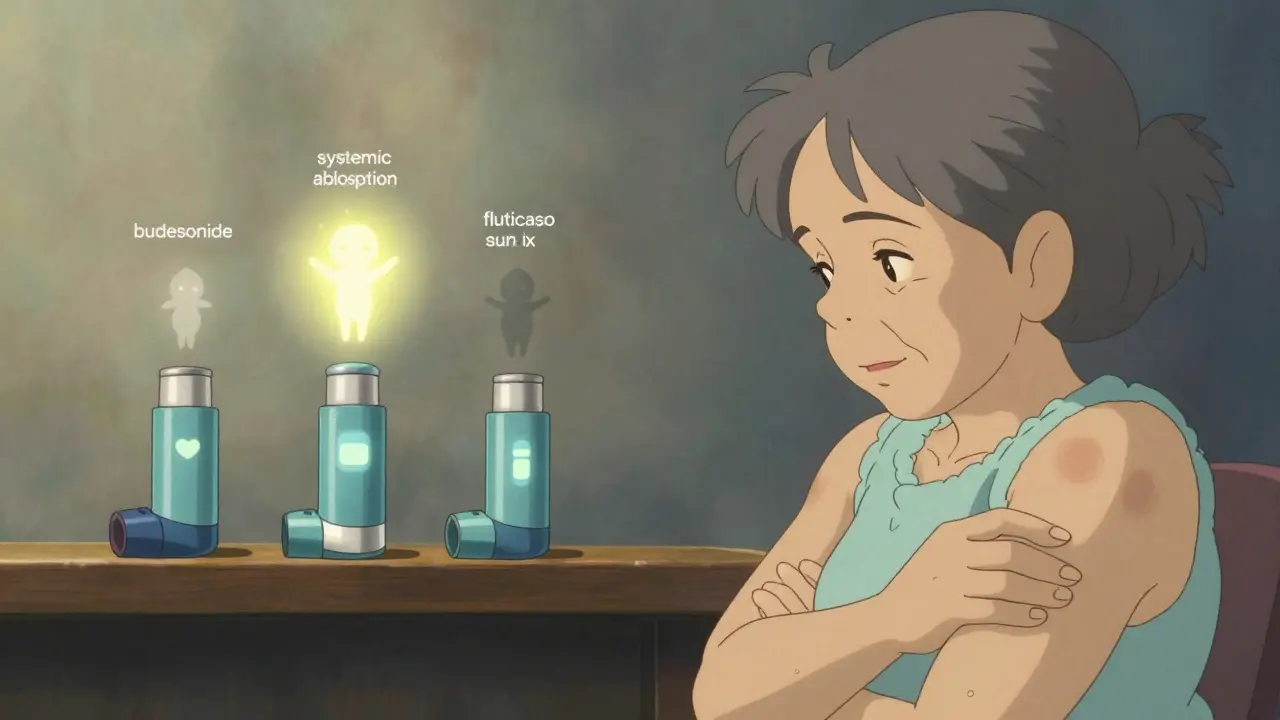
One key thing to remember: the higher the dose, the greater the risk. A 2021 study showed that fluticasone at 500 mcg/day or more had nearly three times the risk of adrenal suppression compared to budesonide at the same dose. That’s not because one drug is "bad"-it’s because different steroids are absorbed differently by your body.
Why Some Inhalers Are Safer Than Others
Not all inhaled steroids are created equal. The amount that escapes your lungs and enters your bloodstream varies dramatically between brands. Here’s how they stack up:
| Medication | Systemic Absorption | Typical Daily Dose (mcg) | Relative Risk of Systemic Side Effects |
|---|---|---|---|
| Fluticasone propionate | 30-40% | 100-500 | High |
| Beclomethasone dipropionate | 20-30% | 200-800 | Moderate |
| Budesonide | 10-15% | 200-800 | Low |
| Mometasone furoate | 10-12% | 100-400 | Low |
| Ciclesonide | 2-3% | 80-320 | Very Low |
Ciclesonide stands out because it’s a prodrug-it only becomes active after it reaches your lungs. Less than 3% enters your bloodstream, making it one of the safest options, especially for long-term use. If you’re on a high dose of fluticasone and experiencing side effects, switching to budesonide or ciclesonide might cut your risk in half without losing control of your asthma.
How to Use Your Inhaler Correctly (And Why It Matters)
Most side effects aren’t caused by the medicine itself-they’re caused by how you use it. If you don’t rinse your mouth, if you don’t use a spacer, or if you don’t inhale deeply enough, up to 80% of the dose lands in your mouth and throat instead of your lungs. That’s not just wasteful-it’s dangerous.
Here’s what actually works:
- Use a spacer with your pressurized inhaler. It holds the medicine in a chamber so you can breathe it in slowly. Studies show this increases lung delivery from 10% to over 60% and cuts throat deposits by 70%. Even a cheap plastic spacer works.
- Rinse and spit after every use. Don’t swallow the rinse water. Just swish with water or mouthwash, then spit it out. This reduces thrush risk by more than half.
- Wait 30 seconds between puffs. If you need more than one puff, wait before taking the next. Rushing means you’re not getting the full dose.
- Check your technique every 3-6 months. A 2021 study found that 45-60% of people using inhalers make at least one major mistake-like not holding their breath after inhaling, or exhaling into the inhaler before use. Your doctor or pharmacist can watch you use it in under two minutes.
Real-world data from Asthma.net shows that people who rinsed after every use cut their thrush risk from 38.7% down to 14.2%. That’s a 63% drop-just from rinsing. And if you’re using a spacer, your risk of voice changes drops from 33% to 11%.
Dose Matters More Than You Think
Many people think: "More medicine = better control." That’s not true with steroids. In fact, once you reach a certain dose, the benefits stop increasing-but the side effects keep climbing.
Experts call this the "sigmoidal curve"-a fancy way of saying the risk doesn’t rise slowly. It explodes after a threshold. Dr. Sally Wenzel, a leading asthma researcher, says: "Below 250 mcg of fluticasone equivalent, side effects are rare. Above 500 mcg, they start rising sharply. At 1000 mcg, you’re essentially getting the same systemic exposure as oral steroids."
The American Academy of Allergy, Asthma & Immunology recommends that if you’ve been on more than 300 mcg/day of fluticasone equivalent for six months or longer, your doctor should check for systemic effects. That means asking about fatigue, bruising, or mood changes-and possibly running a simple blood test for cortisol levels.
Here’s a simple rule: Use the lowest dose that keeps your asthma under control. If you haven’t had a flare-up in six months, talk to your doctor about cutting your dose by 25-50%. Many people can stay symptom-free on half the dose they were on before.
Who Needs Extra Monitoring?
Not everyone needs the same level of check-ups. But some groups are at higher risk:
- Children under 12: Monitor growth every six months. High-dose ICS (>800 mcg/day) increases cataract risk by 2.3 times. Stick to budesonide or ciclesonide if possible.
- Adults over 65: Get a bone density scan if you’ve been on over 750 mcg/day for five years. Watch for bruising or fractures. Pneumonia risk goes up-get your flu and pneumonia vaccines.
- Pregnant people: Budesonide is the safest choice. It’s been studied in over 15 years of pregnancy registries with no increased birth defect risk. Fluticasone is less proven.
- People with diabetes or osteoporosis: These conditions can get worse with long-term steroid use. Your doctor should track your blood sugar and bone health closely.
For elderly patients, a 2023 study found that ICS doses above 500 mcg/day increased fracture risk by 31%. That’s not a small number. It’s the same risk as smoking or being sedentary.

What’s New in Asthma Treatment?
The future of asthma care isn’t just about safer steroids-it’s about moving beyond them. New treatments are changing the game:
- Smart inhalers: These attach to your existing inhaler and track when and how you use it. They catch technique errors with 92% accuracy. If you’re forgetting doses or using it wrong, your doctor gets an alert.
- Blood eosinophil tests: If your eosinophil count is above 300 cells/μL, you might be able to cut your steroid dose in half and still stay in control. This test is now available in most clinics.
- Biologics like dupilumab: For severe asthma, these injectable drugs target specific inflammation pathways. In one trial, they cut ICS use by 70% while improving lung function.
- Ultra-low systemic ICS (like AZD7594): In Phase II trials, this new steroid caused 90% less adrenal suppression than fluticasone. It’s not on the market yet, but it’s coming.
These aren’t science fiction. They’re real, available options-if you know to ask for them.
What to Do If You’re Worried About Side Effects
If you’re on inhaled steroids and you’re experiencing:
- White patches in your mouth
- Unexplained bruising or thin skin
- Constant fatigue or dizziness
- Worsening voice quality
- More frequent infections
Don’t stop your inhaler. That could trigger a serious asthma attack. Instead:
- Start rinsing and using a spacer right away-even if you’ve been using the inhaler for years.
- Ask your doctor for a dose review. Can you go lower? Is there a safer steroid you could switch to?
- Request a cortisol test if you’re on more than 500 mcg/day of fluticasone equivalent and feel tired.
- Get your technique checked. You might be using it wrong without realizing it.
- Ask about biologics or other alternatives if you’re on high doses and still having symptoms.
Most side effects are reversible. Thrush clears up with antifungal mouthwash. Skin thinning improves if you lower your dose. Adrenal function returns once the steroid is reduced. But you need to act-not ignore it.
Final Thought: Control Without Cost
Asthma steroids saved millions of lives. But they’re not harmless. The goal isn’t to avoid them-it’s to use them wisely. You don’t need a high dose to feel safe. You don’t need to live with a hoarse voice or bruised skin. With the right technique, the right dose, and the right monitoring, you can breathe easy without paying the hidden price.
Ask your doctor: "What’s the lowest dose I can stay on?" and "Is there a safer option?" If they don’t know, ask for a referral to an asthma specialist. Your lungs-and your body-deserve more than just a prescription. They deserve a plan.
Can inhaled steroids cause weight gain?
Unlike oral steroids, inhaled corticosteroids rarely cause weight gain. The dose is so low and targeted that it doesn’t trigger the metabolic changes that lead to increased appetite or fat storage. If you’re gaining weight while using an inhaler, it’s more likely due to other factors like reduced activity from asthma symptoms or medications like oral steroids used during flare-ups.
Is it safe to use ICS for years?
Yes, when used at the lowest effective dose. Studies tracking patients for over 20 years show that low-to-moderate doses of budesonide or ciclesonide are safe for long-term use. The key is regular review-every 6-12 months-to ensure you’re not on more than you need. High doses over five years require monitoring for bone, skin, and adrenal health.
Do I need to wean off inhaled steroids?
Only if you’ve been on high doses for a long time and your doctor suspects adrenal suppression. For most people, simply lowering the dose gradually over weeks is enough. Never stop suddenly-this can trigger a life-threatening asthma attack. Always work with your provider to reduce your dose safely.
Can children use ICS safely?
Yes. Standard doses of ICS (under 400 mcg/day beclomethasone equivalent) cause only a small, temporary delay in growth-about 0.7 cm per year-and do not affect final adult height. Budesonide and ciclesonide are preferred in children due to lower systemic absorption. Regular height checks every 6 months are recommended.
What’s the best way to reduce thrush from ICS?
Use a spacer with your inhaler, then rinse your mouth with water and spit it out after every use. Do not swallow the rinse. Brushing your teeth afterward adds extra protection. Studies show this cuts thrush risk by 50-60%. If thrush develops, antifungal mouth rinses (like nystatin) clear it up in 5-7 days.
Are there natural alternatives to inhaled steroids?
There are no proven natural alternatives that match the effectiveness of inhaled corticosteroids for controlling persistent asthma. Supplements like vitamin D or omega-3s may support general lung health but cannot replace anti-inflammatory medication. For people who can’t tolerate steroids, biologic therapies like dupilumab or omalizumab are medically approved alternatives-but they require a prescription and specific asthma triggers.
If you’ve been using your inhaler for more than a year, take a moment today: check your technique, rinse after each use, and ask your doctor if your dose is still right. Small changes make a big difference.


Finally, someone says it. These inhalers are overprescribed. I’ve been on fluticasone for 8 years and I’m bruising like a 90-year-old. My doctor just shrugs and says 'it’s working.' Well, it’s working too well-on my skin, not my lungs.
i never rinse n i still breathe good 😅 but now i will try… thx for the tip
This is such an important post. So many people don’t realize how much technique matters. Using a spacer and rinsing? It’s not optional-it’s part of the treatment. If you’re on steroids long-term, you owe it to yourself to get your technique checked. Your body will thank you.
Let me get this straight-we’re being told to trust Big Pharma’s ‘safer’ steroids while ignoring the fact that ALL steroids are synthetic poisons designed to suppress your body’s natural defenses? Ciclesonide? It’s just a prettier cage. You’re still feeding your lungs chemicals that silence your immune system. What’s next? A steroid lollipop for your kids? This isn’t medicine-it’s chemical surrender.
OMG I just realized I’ve been swallowing my rinse water for 5 years… I’m so embarrassed. I thought it was ‘better’ to swallow it? Like, I didn’t want to waste it?? 😭 I’m switching to a spacer today and rinsing like my life depends on it-because it does. Thank you for this.
Peripheral eosinophil counts are now a critical biomarker for ICS titration. If your eosinophil level is below 300 cells/μL, you’re likely overmedicated. Consider a step-down protocol under supervision-especially if you’ve been stable for >6 months. Biologics should be considered earlier in severe eosinophilic phenotypes.
Wait, so if I rinse after every puff, I cut my thrush risk by 63%? That’s like getting a free vaccine. Why isn’t this on every inhaler box? I feel like I’ve been played.
I’m a 68-year-old with asthma and osteoporosis. I’ve been on fluticasone for 12 years. I never knew my bruising was linked. I got my bone scan last week-T-score of -2.8. I’m switching to budesonide next week. Thank you for giving me the courage to ask my doctor for a change. I didn’t think I had a choice.
STOP. Just stop. If you’re still on high-dose fluticasone and you’re over 60, you’re playing Russian roulette with your bones. I’ve seen three patients break their hips from a fall that should’ve been a stumble. Ciclesonide isn’t ‘new’-it’s common sense. Demand it. Your body isn’t a landfill for pharmaceutical waste.
USA doctors push inhalers like candy. In India, we use nebulizers and Ayurveda for mild cases. Why are you so quick to swallow chemicals? This is not health-it’s profit-driven compliance. You don’t need steroids to breathe. You need better air.
Imagine your lungs as a cathedral-every puff of steroid is a candle, flickering, dimming the light of your own immune fire. We’ve turned breathing into a ritual of chemical supplication. And yet, we call it ‘control.’ What if the real control was listening-to your body, to your breath, to the silence between wheezes? Ciclesonide isn’t safer-it’s a whisper in a world screaming for silence.
Let’s think deeper here. The real issue isn’t the steroid-it’s the entire paradigm of chronic disease management. We’re taught to manage, not to heal. We’re given tools to suppress symptoms, not to address root causes like pollution, stress, or poor nutrition. If we spent half as much money on clean air initiatives as we do on inhalers, we wouldn’t need these drugs at all. The system is designed to keep you dependent-not to cure you. So yes, rinse your mouth, use a spacer, switch to ciclesonide-but also ask: why are we still breathing this air in the first place?