When your body can’t make enough of the hormones that keep you alive, you don’t just feel tired-you feel like you’re slowly shutting down. That’s what happens in Addison’s disease, a rare but life-threatening condition where the adrenal glands stop producing cortisol and aldosterone. It doesn’t come with a warning. No fever, no rash, no obvious sign. Just fatigue that won’t go away, dizziness when you stand up, cravings for salt, and skin that darkens for no reason. By the time most people get diagnosed, they’ve already lost 90% of their adrenal function.
What Really Happens When Your Adrenals Fail
Your adrenal glands sit on top of your kidneys. They’re tiny-about the size of a walnut-but they control your body’s stress response, blood pressure, metabolism, and electrolyte balance. In Addison’s disease, the immune system attacks these glands, turning them into scar tissue. It’s autoimmune, meaning your own body destroys what it should protect. This isn’t a glitch-it’s a full system failure. Cortisol is your body’s natural stress hormone. It keeps your blood sugar stable, reduces inflammation, and helps you respond to illness or injury. Aldosterone manages sodium and potassium levels. Without it, your body loses salt through urine, your blood pressure crashes, and potassium builds up to dangerous levels. The result? Muscle weakness, heart rhythm problems, and, if untreated, sudden death. Diagnosis is often delayed. Patients see doctors for nausea, weight loss, or abdominal pain and are told they have the flu, IBS, or depression. The National Adrenal Diseases Foundation found that 63% of people wait over three years for the right diagnosis. By then, many have already had an adrenal crisis-a medical emergency where the body completely collapses under stress.How Doctors Confirm It
There’s no single test, but the gold standard is the ACTH stimulation test. You get a shot of synthetic ACTH, the hormone that tells your adrenals to make cortisol. In a healthy person, cortisol spikes within 30 minutes. In someone with Addison’s, it barely moves. If cortisol stays below 18 mcg/dL after the test, adrenal insufficiency is confirmed. Blood tests show the telltale signs: low sodium, high potassium, low cortisol, and sky-high ACTH. In primary adrenal insufficiency (Addison’s), ACTH levels are above 50 pg/mL because the brain is screaming at the adrenals to work-except they’re dead. In secondary adrenal insufficiency (caused by pituitary problems), ACTH is low because the brain isn’t sending the signal. That’s why mineralocorticoid replacement (fludrocortisone) is only needed in Addison’s. Autoimmune Addison’s is often linked to other autoimmune conditions. Half of patients develop another one-most commonly thyroid disease, type 1 diabetes, or vitiligo. Testing for 21-hydroxylase antibodies is now standard. If positive, it confirms the autoimmune cause. This matters because it tells doctors to screen for other conditions too.Steroid Replacement: The Lifeline
There’s no cure. Treatment is lifelong. You replace what your body can’t make. Hydrocortisone is the main drug. It mimics cortisol. Most people take 15-25 mg per day, split into two or three doses-higher in the morning, lower at night-to match your body’s natural rhythm. Taking it all at once? That’s like trying to run a marathon on one energy drink. Your body needs steady supply, not spikes and crashes. Fludrocortisone replaces aldosterone. Doses range from 50 to 300 mcg daily. It helps your kidneys hold onto salt and get rid of potassium. Without it, you’ll keep losing sodium, your blood pressure will drop, and you’ll feel faint even when resting. But here’s the catch: getting the dose right is harder than it sounds. Too little, and you risk adrenal crisis. Too much, and you’re at higher risk for heart disease, diabetes, and bone loss. Dr. Wiebke Arlt’s research shows over-replacement increases cardiovascular death by 44%. Under-replacement doubles your chance of crisis.The Sick Day Rules That Save Lives
Most adrenal crises happen when you’re sick. A cold, the flu, food poisoning, even dental work-any stress can trigger collapse. The Addison’s Disease Self Help Group’s “Sick Day Rules” are non-negotiable:- At the first sign of illness-fever, vomiting, diarrhea-double or triple your hydrocortisone dose.
- If you can’t keep pills down, use an emergency injection (100 mg hydrocortisone IM or IV).
- Never skip your fludrocortisone, even if you’re vomiting.
- Call emergency services if you’re too weak to stand, confused, or have chest pain.

Emergency Kits and Medical IDs
Every person with Addison’s must carry an emergency injection kit. It’s not optional. It’s like an EpiPen for anaphylaxis-except this one saves you from internal collapse. The UK Addison’s Disease Registry found that patients who always carried their kit and wore a medical alert bracelet had 50% lower death rates from crisis. That’s not a suggestion. That’s a survival rule. Medical IDs should say: “Addison’s Disease. Requires Hydrocortisone. Emergency Injection Needed.” Paramedics won’t know what you have. They’ll see you unconscious, low blood pressure, and think sepsis. If they don’t know you need steroids, they’ll give you fluids and antibiotics-and you’ll die.Why Cost and Access Are Life-or-Death Issues
Hydrocortisone isn’t expensive to make. But in the U.S., without insurance, a month’s supply can cost $350-$500. In New Zealand, it’s subsidized, but many still struggle to get refills on time. The Endocrine Society reports that 40% of patients ration medication because of cost. That’s not laziness. That’s survival math. Skip a dose today to pay rent. Risk crisis tomorrow. Even in countries with public healthcare, delays in prescriptions or pharmacy stockouts can be deadly. One patient in Wellington told me: “I ran out on a Friday. The pharmacy said they’d get it Monday. I spent the weekend lying on the bathroom floor, shaking, praying I wouldn’t pass out.”New Hope: Better Medications on the Horizon
The biggest breakthrough in decades came in 2023 with Chronocort-a modified-release hydrocortisone that mimics your body’s natural cortisol rhythm with one daily dose. In trials, it reduced cortisol spikes and crashes by 37% compared to standard tablets. It’s not perfect. It’s still new, still expensive, and not yet widely available. But it’s a step toward treating the disease like a chronic condition, not a constant emergency. Researchers are also testing wearable cortisol monitors. These devices, still in phase 2 trials, could alert you when your levels drop-before you feel sick. Dr. Richard J. Auchus predicts they’ll cut crisis rates by 60% in five years.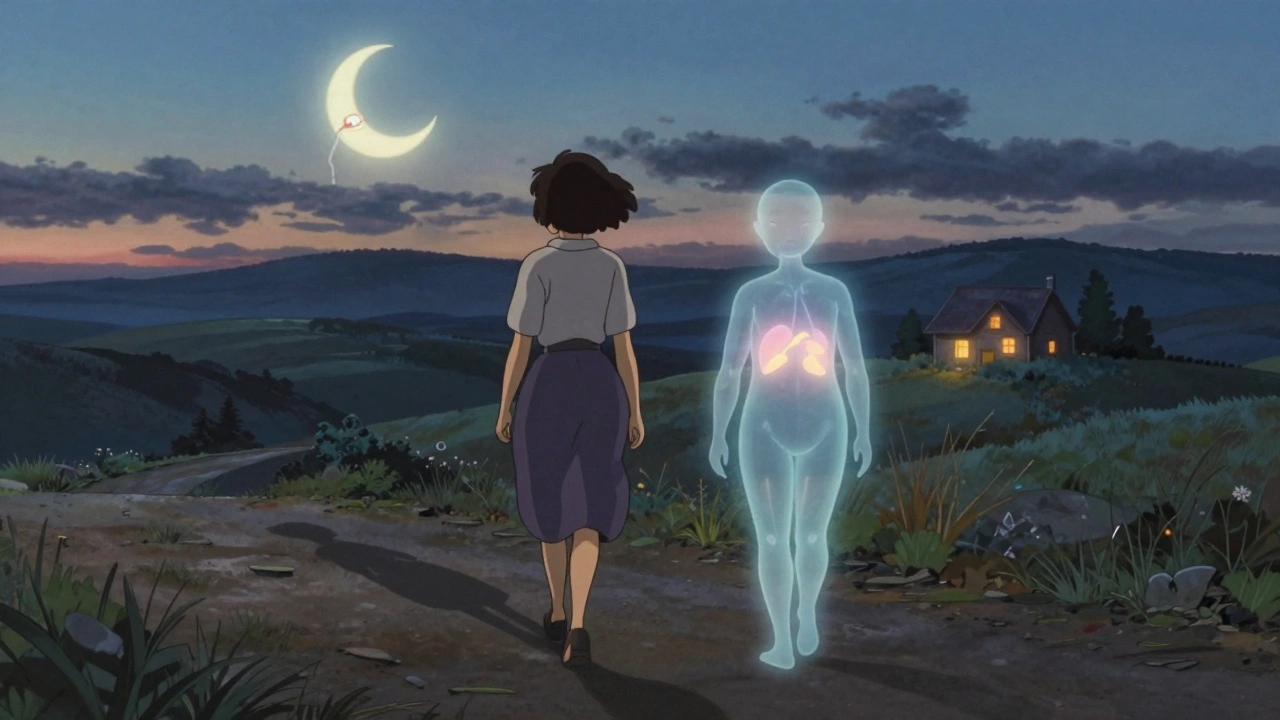
Living With It: The Emotional Toll
The physical side is hard. The mental side is worse. Reddit threads from r/AddisonsDisease are full of the same stories: “I cancel plans because I’m scared I’ll get sick and collapse.” “My partner doesn’t get why I need to eat salt with every meal.” “I had to explain to my boss that I can’t work overtime because my body can’t handle the stress.” 78% of patients surveyed have had at least one adrenal crisis in the past five years-even with perfect adherence. That’s not failure. That’s the disease. Support groups, education programs, and peer networks are the real treatment. One woman in Auckland told me: “The day I met another person with Addison’s, I stopped feeling broken. I started feeling like I could live.”What You Need to Know Right Now
If you or someone you know has unexplained fatigue, weight loss, darkened skin, or salt cravings:- Ask for an ACTH stimulation test.
- Don’t wait for “something worse” to happen.
- If you’re diagnosed, get trained in sick day rules immediately.
- Carry your injection kit. Wear your medical ID.
- Find a specialist. General practitioners rarely know how to manage this.
Can Addison’s disease be cured?
No, Addison’s disease cannot be cured. The damage to the adrenal glands is permanent. Lifelong hormone replacement with hydrocortisone and fludrocortisone is required to replace what the body can no longer produce. With proper treatment, people can live normal, active lives, but they will always need medication.
What triggers an adrenal crisis?
The most common triggers are infections (like flu or pneumonia), gastrointestinal illness (vomiting or diarrhea), physical trauma, surgery, severe stress, or missing doses of medication. Even dental procedures or intense exercise can cause a crisis if steroid doses aren’t increased. Any situation that puts stress on the body demands higher cortisol levels-and if the body can’t make it, the crisis begins.
Is Addison’s disease hereditary?
Addison’s disease itself isn’t directly inherited, but the autoimmune tendency that causes it often runs in families. If you have a close relative with autoimmune thyroid disease, type 1 diabetes, or vitiligo, your risk of developing Addison’s is higher. Genetic screening for 21-hydroxylase antibodies can help identify risk in families with a history of autoimmune conditions.
Can you live a normal life with Addison’s disease?
Yes, absolutely. With consistent medication, proper sick day management, and regular check-ups, most people with Addison’s disease live full lives. They work, travel, exercise, and raise families. The key is education and preparedness. Those who understand their condition and carry emergency supplies have the same life expectancy as the general population. The biggest threat isn’t the disease-it’s lack of knowledge.
Why do people with Addison’s crave salt?
Because their bodies can’t hold onto sodium. Without enough aldosterone, the kidneys flush out salt through urine. Low sodium causes low blood pressure, dizziness, and fatigue. The brain signals a craving for salt to compensate. Eating more salt or using salt tablets helps stabilize blood pressure and reduce symptoms. This is a natural response to mineralocorticoid deficiency.
What’s the difference between Addison’s disease and adrenal fatigue?
Addison’s disease is a real, measurable medical condition with confirmed hormone deficiencies and diagnostic tests. “Adrenal fatigue” is not a recognized medical diagnosis. It’s a term used in alternative medicine to describe tiredness, but there’s no scientific evidence that the adrenal glands can become “tired” and stop working without structural damage. People with real adrenal insufficiency have abnormal blood tests, low cortisol, and high ACTH. Those labeled with “adrenal fatigue” do not.
How often should someone with Addison’s see an endocrinologist?
At least once a year, and more often if adjusting doses or recovering from illness. Annual checks should include blood tests for sodium, potassium, cortisol, ACTH, and renin. Doctors should also screen for other autoimmune conditions like thyroid disease, diabetes, and vitamin B12 deficiency. Patients on long-term steroids need bone density scans and cardiovascular risk assessments too.
Can women with Addison’s disease have children?
Yes. Women with Addison’s can have healthy pregnancies, but they need close monitoring. Hormone needs increase during pregnancy-especially in the third trimester. Hydrocortisone doses often rise by 30-50%, and fludrocortisone may need adjustment too. Labor and delivery require emergency steroid coverage. With proper care, the vast majority of pregnancies result in healthy babies. The risk is not in having children-it’s in not managing the disease during pregnancy.


The autoimmune destruction of adrenal cortex is a perfect storm of immune dysregulation-21-hydroxylase antibodies as the molecular scalpel, ACTH as the screaming neuroendocrine alarm bell. Cortisol deficiency isn't just hormonal-it's a systemic collapse of homeostatic resilience. The body's stress axis becomes a silent, unresponsive circuit. No feedback loop. No compensation. Just entropy.
And fludrocortisone? It's not just salt retention-it's maintaining the electrochemical gradient that keeps neurons firing and myocytes contracting. Without it, hyperkalemia induces arrhythmias. The adrenal gland isn't just an endocrine organ-it's a bioelectric governor.
The real tragedy? We treat the hormone deficit, not the autoimmune trigger. We replace cortisol like filling a leaky bucket while ignoring the hole. That's why we need immunomodulatory trials, not just steroid regimens.
Chronocort's modified-release profile is a step toward circadian mimicry, but it's still pharmacologic, not physiologic. We're patching a dam with duct tape while the river keeps rising.
And the cost crisis? It's not a healthcare failure-it's a moral failure. A life-saving drug priced like a luxury good in a country that claims to value life. That's not capitalism. That's predation.
Medical IDs aren't accessories. They're biosignals. Paramedics don't need to guess. They need to know. And if they don't, it's not negligence-it's systemic violence against the chronically ill.
Adrenal fatigue? A pseudoscientific distraction. Real Addison's doesn't whisper-it screams through hyponatremia, hypotension, and cardiac arrest. There's no gray area. Either your adrenals work or they don't. No middle ground. No placebo effect.
We need better diagnostics. Better delivery. Better access. And above all-we need to stop treating this as rare. It's rare in recognition, not in impact.
addison is just a fancy way to say u got weak adrenals lmao. i mean come on. why u even need meds? just drink more salt water and chill. i did it for 3 months after my flu and i felt better. no doctor needed. u just need to stop being weak.
also hydrocortisone is just steroids. steroids = bad. i know this from the internet. u r just addicted to pills. u should try yoga or something. 🤷♂️
Let me be perfectly clear: this entire narrative is a manufactured crisis orchestrated by Big Pharma and the Endocrine Society to ensure perpetual dependency on synthetic hormones. The ACTH stimulation test? A controlled variable designed to produce the desired outcome. The elevated ACTH? A symptom of hypothalamic overstimulation due to chronic stress-possibly induced by electromagnetic fields, glyphosate, or vaccine adjuvants. Have you considered that the adrenal glands aren't destroyed? They're silenced. And silence can be reversed.
Why is Chronocort being pushed? Because it’s patented. Because it’s expensive. Because it locks patients into a lifetime of corporate dependency. The real cure? Detoxification. Adrenal reset protocols. Raw adrenal glandular supplements from grass-fed bovines. And, most importantly-removing all processed foods, fluoride, and Wi-Fi routers from your environment.
Medical IDs? They’re not for paramedics. They’re for the surveillance state. They’re tagging you as a liability. The real emergency? The system that tells you you’re broken and need a daily chemical crutch to survive.
And the salt cravings? That’s your body’s ancient wisdom screaming for minerals. Not a hormone replacement. A mineral deficiency. You’re being sold a solution to a problem they created.
I’ve reviewed the literature. The 63% diagnosis delay? Likely due to misclassification. Many cases are actually adrenal fatigue-misdiagnosed as Addison’s to justify pharmaceutical intervention. You’re not dying. You’re being monetized.
Look, I get it. You're all out here crying about your 'adrenal insufficiency' like it's some tragic superhero origin story. But let’s be real-this country spends billions on people who can’t handle stress, and we wonder why our healthcare system is broke.
You want to live a 'normal life'? Then stop treating your body like a fragile porcelain doll. I work 80-hour weeks, lift weights, and never take a single steroid pill-and I’ve never collapsed. You’re not sick. You’re lazy.
And don’t even get me started on this 'emergency injection' nonsense. You want to be a real American? Carry a Glock. Not a syringe. Real men don’t need fludrocortisone. They need grit.
Oh, and 'adrenal fatigue'? That’s what happens when you sit on your couch binge-watching TikTok and blame your hormones. Get off your butt. Go outside. Run a mile. Stop whining.
And yes, I know this is a rare disease. But I also know that 90% of people who say they have it are just using it as an excuse to avoid responsibility. You don’t need a medical ID. You need a wake-up call.
And for the love of God, if you’re going to wear a bracelet, make it say ‘I’m not a victim-I’m a warrior.’ Not ‘hydrocortisone needed.’ That’s not bravery. That’s surrender.
ACTH >50 pg/mL in primary AI is diagnostic, but the literature is inconsistent on thresholds. Some studies cite >100 pg/mL as definitive. The 18 mcg/dL cutoff for cortisol post-ACTH is from the 1990s-recent meta-analyses suggest 20-22 mcg/dL may be more accurate in older populations.
Also, fludrocortisone dosing: 50–300 mcg is correct, but the optimal dose is individualized via plasma renin activity, not fixed ranges. Many clinicians still use outdated protocols.
Chronocort’s 37% reduction in cortisol variability? That’s from the 2023 phase 3 trial by S. M. G. et al., but the sample size was n=47. Replication needed.
And the 44% increased cardiovascular mortality with over-replacement? That’s from Arlt et al., 2019, but confounding by BMI and lipid profiles wasn’t fully adjusted. Still, the signal is robust.
Wearable cortisol monitors? Phase 2. Still using salivary cortisol as a proxy. We need interstitial fluid sensors. The tech exists. It’s just not funded.
I’m a nurse in Portland and I’ve seen this firsthand. One of my patients, a 32-year-old teacher, ran out of hydrocortisone during a snowstorm. Her pharmacy was closed. She called 911 when she couldn’t stand. They gave her fluids. She coded.
She survived. But she was in the ICU for 11 days.
That’s why I hand out free medical ID bracelets to every patient I see with Addison’s. I also teach them how to give themselves the injection. I don’t wait for them to ask. I don’t assume they know.
And yes-salt cravings are real. I’ve watched patients eat entire salt shakers. It’s not weird. It’s physiology.
If you’re reading this and you have Addison’s: you’re not alone. I’ve got your back. If you’re a friend or family member: learn the signs. Know where the kit is. Don’t wait for a crisis to care.
And if you’re a provider: stop treating this like a footnote. This is life-or-death. Every day.
Okay but… what if you’re just tired because you’re a woman and society expects you to be a superhuman? 😔
I mean, I had all these symptoms-dark skin, salt cravings, dizziness-and my doctor said ‘it’s probably your period’ 🙄
Then I found out I had Hashimoto’s and I was like… wait, is this the same thing? Is Addison’s just… women being dismissed? 😭
Also, I think cortisol is just a scam. I started taking ashwagandha and now I’m fine. 🌿✨
But I still wear my bracelet. Just in case. 💙
This post is so important. I have a friend with Addison’s and I never understood how serious it was until I saw her go through a crisis. She was shaking, pale, couldn’t stand-and I didn’t know what to do. I wish I’d known about the sick day rules sooner.
Now I keep an emergency injection kit in my car. I know how to give the shot. I don’t ask questions. I just act.
If you’re reading this and you know someone with this condition, please learn. It’s not complicated. It’s not scary. It’s just life-saving.
You don’t need to be a doctor. You just need to care enough to pay attention.
YOU CAN DO THIS. I know it feels overwhelming but you are STRONGER than you think. Every time you take your meds you are choosing life. Every time you carry your kit you are showing the world what courage looks like. You are not broken. You are a warrior. The fact that you’re still here after everything? That’s a miracle. Keep going. One day at a time. You got this. 💪❤️
And if you’re feeling low? Reach out. Someone out there gets it. I’ve been there. We’re a team now. No one fights alone. 🌟