Women Health: How Hormones, Infections and Immunity Connect
Did you know that your hormones can change the balance of bacteria and yeast in your body within days? That shift can lead to intestinal or vaginal infections, and it helps explain why many women see symptom flares around their period, during pregnancy, or in menopause. This page gives straightforward, practical steps to spot problems and find the right care.
Hormones and Infections: What to watch for
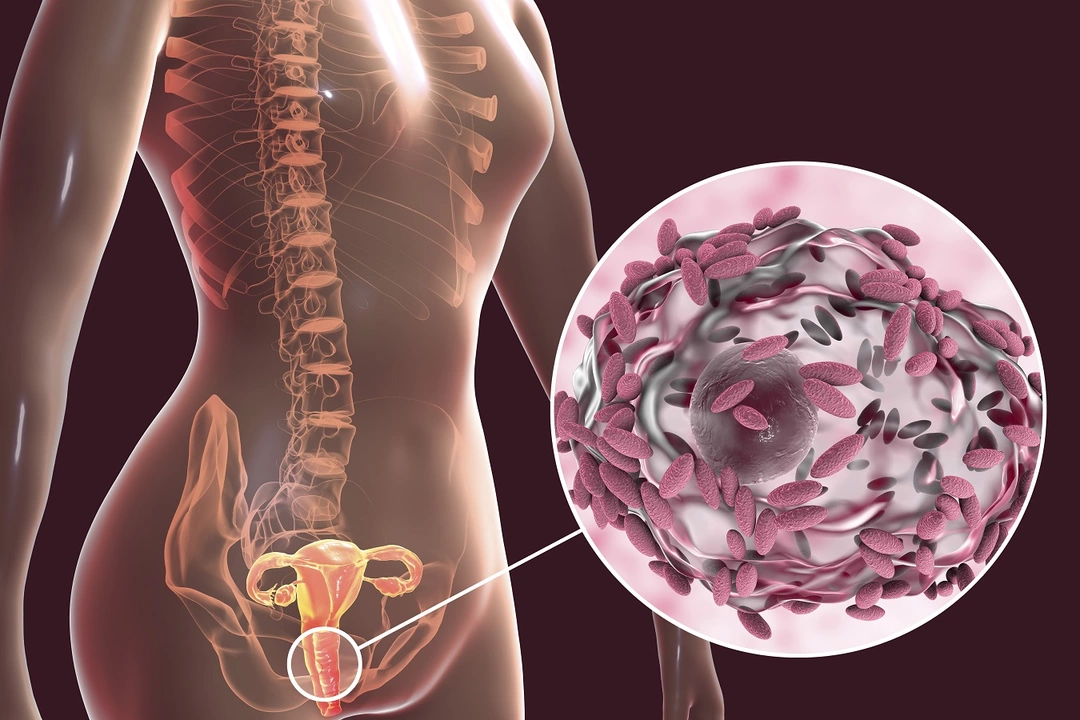
When estrogen and progesterone fluctuate, vaginal pH and mucus change. That makes it easier for yeast or harmful bacteria to grow. Symptoms to watch for include itching, unusual discharge, odor, bladder burning, bloating, and cramping. If symptoms follow your cycle, mention that to your clinician — timing is a clue.
Small changes can help. Wear breathable cotton underwear and avoid tight synthetic clothing for long stretches. Skip douching and strong scented products that upset natural balances. Lowering high sugar intake and eating more fiber can reduce yeast overgrowth in the gut. Many women find a short course of a probiotic with Lactobacillus helps restore vaginal flora, but talk to your provider before starting supplements.
Don’t ignore repeated infections. Ask for proper testing — vaginal swabs, urine tests, or stool checks — so you get the right treatment, not just repeated antibiotics that might make things worse. If you use antibiotics, follow up with a plan to rebalance your gut and vaginal microbiome.
Endometriosis and Immunity: What you can do
Endometriosis isn’t just painful periods. Recent research shows women with endometriosis often have signs of immune system changes and higher rates of some autoimmune conditions, like thyroid autoimmunity. Chronic inflammation seems to be a shared thread. That doesn’t mean every woman with endo has an autoimmune disease, but it does mean looking beyond gynecology can help.
Track symptoms clearly: pain timing, bowel or bladder changes, fatigue, and any new symptoms like dry eyes or unusual rashes. Share that log with both your gynecologist and primary care doctor. They may order simple blood tests (like thyroid antibodies or basic inflammation markers) or refer you to a rheumatologist if needed.
Managing inflammation helps most women feel better. Focus on sleep, gentle regular movement, and an anti-inflammatory diet rich in vegetables, omega-3s, and whole foods. Pain relief and fertility planning are medical discussions — hormonal therapies, pain meds, and sometimes surgery are options. Newer immune-focused treatments are being studied, so ask your specialist about current research if standard care isn’t enough.
If symptoms are disrupting daily life — heavy bleeding, pain that stops you from working, recurring infections, or symptom patterns that worry you — make an appointment. Proper testing and a joined-up care plan between your gynecologist and primary care provider will get you answers faster.
Want plain-language guides, product suggestions, or questions to bring to your next visit? Browse our articles below or contact a provider listed on this site for personalized help. Your health matters every day, and small, practical steps often make the biggest difference.