Vaginal infections: quick help, causes, and when to get care
About three in four women will have a yeast infection at some point. That shows how common vaginal infections are—and how confusing they can be. Symptoms overlap, so knowing the key signs helps you choose the right care fast.
Common causes & symptoms
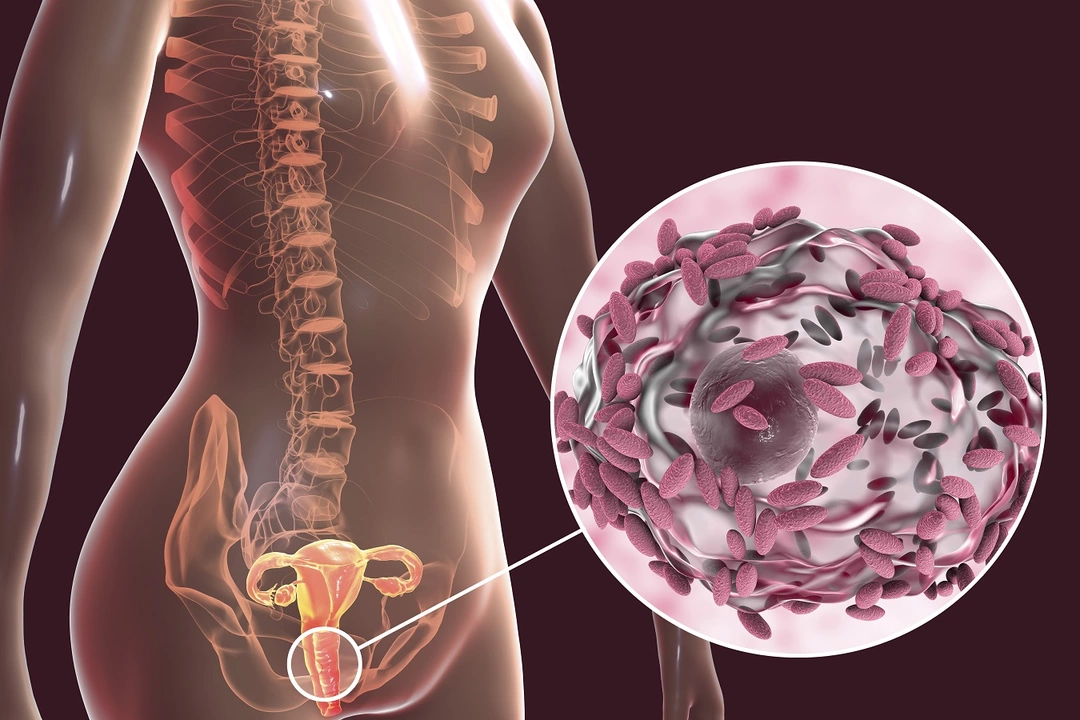
There are three main problems you’ll see: yeast infection (Candida), bacterial vaginosis (BV), and trichomoniasis. Yeast usually gives thick white cottage-cheese discharge, intense itching, and burning. BV makes a thin grayish or white discharge with a fishy smell, especially after sex. Trichomoniasis often causes frothy, yellow-green discharge and heavy irritation. Urinary symptoms or pelvic pain suggest something more serious and need urgent care.
Risk factors matter. Antibiotics, high blood sugar, pregnancy, hormonal birth control changes, and tight synthetic underwear all raise the chances of infection. Douching destroys healthy bacteria and increases risk—skip it.
What to do and when to see a doctor
If you suspect a yeast infection and you’ve had one before, an over-the-counter antifungal cream or single-dose pill often works. Follow the package directions. If symptoms improve in 48–72 hours, keep using the full course. If nothing gets better, stop guessing and see a clinician.
See a doctor right away if you have a fever, severe pain, heavy bleeding, a very bad odor, or if you are pregnant. Also see care if this is your first infection, you get recurrent infections (four or more a year), or you have diabetes or a weakened immune system. A clinician may do a swab, look under a microscope, or order tests to find the exact cause.
Treatment varies: antifungal drugs for yeast, metronidazole or clindamycin for BV, and a specific antibiotic for trichomoniasis. Don’t share meds or use leftover prescriptions; wrong treatment can make things worse.
Simple self-care helps a lot. Wear cotton underwear, avoid tight pants, wipe front to back, and change wet bathing suits quickly. Use mild, fragrance-free soap and skip scented tampons, pads, and sprays. Probiotics with Lactobacillus may help restore balance, but pick products with proven strains and talk to your provider first.
Recurrent infections deserve a plan. Your clinician might check for diabetes, adjust birth control, or prescribe longer antifungal therapy. If partners are involved, sometimes treating them reduces reinfection risk.
If you’re sexually active, partners may need testing. Use condoms until treatment is done. Avoid OTC home remedies like boric acid without guidance; it can burn. For recurring yeast infections, a test for Candida species can guide treatment—some strains need longer therapy. Keep a symptom diary noting timing, menstrual cycle, sex, and medications; that helps your clinician find triggers faster. Call your clinic if symptoms worsen.
Quick tip: if the discharge smells strongly fishy and becomes worse after sex, think BV. If itching and thick white clumps dominate, think yeast. When in doubt, testing avoids wrong treatment.
Knowing the signs, avoiding risky habits, and getting timely care keep problems short and simple. You don’t have to suffer—get checked when things feel off.