Cholesterol Lowering Exercise Calculator
Your Cholesterol Improvement Estimate
Projected LDL Reduction:
-4.9 mg/dL
Projected HDL Increase:
+2.6 mg/dL
Estimated Timeframe: 3 months of consistent exercise
Recommendation: Combine with a heart-healthy diet for maximum benefit
How This Works
Based on research showing that:
- 150 minutes/week of moderate activity lowers LDL by ~4.9 mg/dL
- 75 minutes/week of vigorous activity lowers LDL by ~7 mg/dL
- Regular strength training increases HDL by ~3 mg/dL
Your personalized estimate combines these effects based on your inputs.
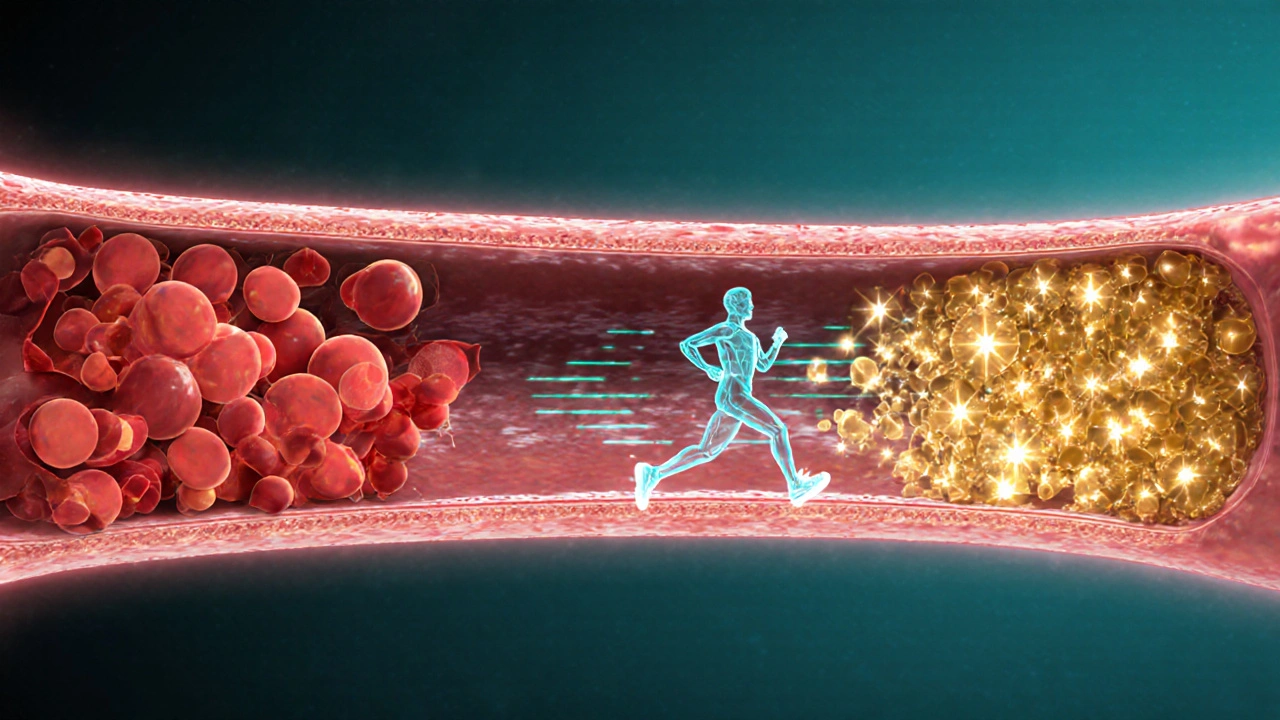
When your blood test shows a cholesterol number that’s creeping up, the usual advice is to reach for a pill. But there’s a free, side‑effect‑free tool that can shift those numbers in a good direction: physical activity. Regular movement not only burns calories, it tweaks the chemistry of your blood, boosting the “good” cholesterol and trimming the “bad” kind. Below, we break down why exercise works, which workouts give the biggest payoff, and how to fit them into a busy life.
Key Takeaways
- Moderate‑intensity exercise can raise HDL (the "good" cholesterol) by 5‑10% in a few months.
- Vigorous activities like running or cycling lower LDL (the "bad" cholesterol) by 3‑7% when done 3‑5 times a week.
- The World Health Organization (2024) still recommends at least 150minutes of moderate or 75minutes of vigorous activity per week for cholesterol control.
- Combining cardio with resistance training yields the strongest effect on lipid profiles.
- Small habits - brisk walks after meals, stair‑climbing, weekend hikes - add up to big heart‑health gains.
Physical activity is a movement that expends energy, ranging from walking to high‑intensity interval training, and influences many metabolic pathways. High blood cholesterol refers to elevated levels of low‑density lipoprotein (LDL) and total cholesterol in the bloodstream, a major risk factor for cardiovascular disease. Understanding how these two interact is the first step toward better heart health.
How Exercise Changes Cholesterol Chemistry
Three biological mechanisms explain the cholesterol‑lowering power of regular exercise:
- Enzyme activation: Physical activity boosts the activity of lipoprotein lipase (LPL), an enzyme that clears triglyceride‑rich particles from the blood and facilitates the conversion of LDL to HDL.
- Weight management: Weight management the process of maintaining a healthy body weight through diet and activity reduces visceral fat, which releases fewer inflammatory cytokines that otherwise raise LDL.
- Improved insulin sensitivity: Regular movement makes cells respond better to insulin, lowering insulin spikes that can drive excess cholesterol production.
These changes translate into measurable shifts in blood markers. A 2023 meta‑analysis of 55 trials found that participants who added 150minutes of moderate exercise per week lowered LDL by an average of 4.9mg/dL and raised HDL by 2.6mg/dL after three months.
Exercise Types and Their Impact on Lipids
| Activity | Intensity | LDL Change | HDL Change |
|---|---|---|---|
| Brisk walking | Moderate (3‑4mph) | -3mg/dL | +2mg/dL |
| Jogging / running | Vigorous (6‑8mph) | -7mg/dL | +5mg/dL |
| Cycling (outdoor) | Moderate‑vigorous | -5mg/dL | +4mg/dL |
| Resistance training | Moderate (8‑12 reps) | -2mg/dL | +3mg/dL |
| HIIT (high‑intensity intervals) | Very vigorous (30s bursts) | -6mg/dL | +6mg/dL |
Notice that activities that raise the heart rate for longer periods-like jogging or HIIT-tend to produce the biggest LDL drops, while any consistent cardio raises HDL. Pairing cardio with a couple of resistance sessions each week maximizes both lipid improvements and muscle mass, which further supports metabolic health.
How Much Exercise Is Enough?
The 2024 WHO guidelines still serve as the baseline:
- At least 150minutes of moderate‑intensity aerobic activity per week (e.g., brisk walking, light cycling), or 75minutes of vigorous‑intensity (e.g., running, HIIT).
- Include muscle‑strengthening activities on 2 or more days per week.
- Spread sessions throughout the week; 30‑minute bouts are easiest to stick with.
If your primary goal is cholesterol control, aim for the higher end of these ranges. A practical schedule might look like:
- Monday - 30min brisk walk + 20min body‑weight circuit.
- Wednesday - 25min cycling (moderate) + 15min dumbbell rows.
- Friday - 20min HIIT (30‑second sprints) + 10min core work.
- Saturday - 45‑min hike (moderate‑vigorous).
That adds up to roughly 150minutes of moderate‑to‑vigorous cardio plus two strength days, a routine shown to shave 5‑10mg/dL off LDL in three months.

Making Exercise Stick - Real‑World Tips
Consistency beats intensity for most people. Here are habits that turn “I’ll start next week” into a daily habit:
- Schedule it: Put workouts on your calendar like any other appointment.
- Link to a daily cue: Walk the dog right after lunch, or do a 10‑minute stretch after brushing your teeth.
- Use technology wisely: A simple step‑counter or heart‑rate monitor can give instant feedback and keep you in the target zone.
- Mix pleasure with purpose: Choose activities you enjoy-dance classes, team sports, or a scenic bike ride-to boost adherence.
- Track progress: Record your cholesterol numbers every 3‑6months; seeing the drop fuels motivation.
Remember, any movement is better than none. Even a 10‑minute stair climb after dinner can spark the enzymatic changes we discussed earlier.
Potential Pitfalls and How to Avoid Them
Many people stumble when trying to use exercise for cholesterol management. Common mistakes include:
- Doing too much, too soon: Jumping into marathon training can lead to injury and burnout. Build weekly volume gradually (5-10% increase per week).
- Ignoring diet: Exercise won’t fully offset a diet high in saturated fats and trans‑fats. Pair workouts with a Mediterranean‑style eating plan for best results.
- Skipping strength work: Pure cardio improves HDL, but without resistance training you miss out on muscle‑mass gains that aid insulin sensitivity and basal metabolic rate.
- Not monitoring intensity: Staying in the “talk test” zone (moderate) is essential for the cholesterol benefit; overly leisurely walks may fall short.
- Overreliance on supplements: Some over‑the‑counter products claim to boost HDL. Evidence is weak; focus on proven lifestyle changes instead.
Address these early, and you’ll keep the momentum while your blood work improves.
Frequently Asked Questions
Can walking really lower my LDL?
Yes. A 2022 study of 1,200 adults showed that a 30‑minute brisk walk five days a week reduced LDL by an average of 3mg/dL after 12 weeks, without any dietary changes.
How fast will I see changes in my cholesterol numbers?
Most people notice a measurable shift after 8‑12 weeks of consistent activity. Blood tests taken every three months are ideal for tracking progress.
Do I need a gym membership?
Not at all. Home‑based cardio (jump rope, body‑weight circuits) and outdoor options (walking, cycling) provide the same lipid benefits as a treadmill or elliptical.
Is there a risk of lowering HDL too much?
Unlikely. Exercise typically raises HDL or keeps it stable. Very extreme endurance training can modestly reduce HDL, but this occurs only in elite athletes training >10hours per week.
Should I combine exercise with cholesterol‑lowering medication?
Absolutely. Medications like statins work via a different pathway (inhibiting HMG‑CoA reductase). Adding regular activity can enhance overall risk reduction by about 15‑20% compared to medication alone.
Bottom line: regular physical activity isn’t just a weight‑loss trick-it’s a proven, cost‑free medicine for high cholesterol. By choosing the right mix of cardio and strength, logging your sessions, and pairing them with a heart‑healthy diet, you can nudge your lipid profile into a safer zone and lower your risk of cardiovascular disease.


Reading through the breakdown really made me think about how intertwined our daily habits are with heart health. It’s amazing how a simple 30‑minute walk can set off a cascade of enzymatic changes that benefit cholesterol. I’ve started pairing my evening walks with a few body‑weight exercises and have already seen a small boost in my energy levels. If you stay consistent, the chemistry will gradually shift – patience is key. Keep at it, and remember that every step counts toward a healthier future.
All this “exercise cures everything” hype is just a cover‑up for the pharma agenda, mate.
While the article is comprehensive, I noticed a small grammatical oversight: the phrase "weight management the process" should be "weight management, the process." Such minor errors can distract readers from the otherwise solid content. Nonetheless, the data cited from the 2023 meta‑analysis is spot‑on and provides a clear quantitative framework. I appreciate the balanced discussion of both cardio and resistance training, as many sources tend to overemphasize one over the other.
I agree with the balanced approach and think scheduling workouts helps a lot
Yo folks! 🚀 Let’s get moving and smash those cholesterol numbers! Even a quick 10‑minute HIIT burst can fire up your metabolism and knock LDL down fast. Pair that with a couple of push‑up sessions and you’re basically giving your heart a high‑five. Remember, consistency beats intensity – so set a reminder, grab a buddy, and make it fun! 🌟 Your blood work will thank you in a few months!
Great points, Rushikesh! 👍 Regular activity truly triggers LPL activity, which clears triglycerides efficiently. Just a heads‑up: the article mentions “weight management the process” – a tiny typo, but the message is crystal clear. Keep the momentum and maybe sprinkle in some yoga for flexibility! 🧘♂️
For those considering integrating exercise into cholesterol management, I recommend setting SMART goals: Specific, Measurable, Achievable, Relevant, and Time‑bound. For instance, target a 150‑minute weekly moderate‑intensity schedule and log your sessions in a journal. Review lipid panels every three months to observe trends, and adjust intensity accordingly. This structured approach aligns clinical evidence with personal accountability.
Alright, let’s talk about why the whole “exercise is the miracle cure” narrative is both overhyped and, frankly, a bit lazy on the part of health writers. First, the data presented in the article, while solid, neglects to mention the variance among individuals – not everyone sees a 5‑mg/dL drop in LDL with the same regimen, which is a fundamental truth often omitted. Second, there’s an implicit assumption that readers have unrestricted access to safe environments for walking, jogging, or HIIT, ignoring socioeconomic barriers that can stifle adherence; this omission subtly shifts responsibility onto the patient without acknowledging systemic challenges. Third, the piece briefly touches on diet but fails to delve into the synergistic effects of nutrition and exercise, leaving the impression that cardio alone can offset a diet high in saturated fats, which is misleading. Fourth, while the article cites a 2023 meta‑analysis, it does not discuss the quality of the underlying studies – many had short durations, small sample sizes, or were funded by fitness industries, raising questions about potential bias. Fifth, the recommendation to “schedule it like any other appointment” can sound simple, yet for individuals with chronic conditions, caregiving responsibilities, or shift work, such scheduling is far from trivial. Sixth, the emphasis on the 150‑minute weekly target, though aligned with WHO guidelines, doesn’t account for the diminishing returns observed in high‑intensity interval training beyond a certain point, which may lead some readers to overtrain and risk injury. Seventh, the article’s tone is overly optimistic, promising measurable blood‑work changes after 8‑12 weeks, whereas real‑world outcomes often show modest improvements that need sustained effort over years. Eighth, the brief mention of strength training’s impact on HDL could have been expanded to discuss how increased muscle mass boosts basal metabolic rate, indirectly influencing lipid metabolism. Ninth, there’s a glaring absence of discussion about how stress management, sleep quality, and mental health intersect with cholesterol levels – all crucial components of a holistic approach. Tenth, the user interface of the calculator is nice, but it lacks transparency about the algorithmic assumptions, leaving users to trust a “black box” without understanding the underlying model. Eleventh, the article could benefit from more diverse examples, such as incorporating culturally relevant activities like dance, rowing, or traditional games, to broaden accessibility. Twelfth, while the author mentions “any movement is better than none,” this statement undermines the importance of progressive overload for measurable physiological adaptation. Thirteenth, readers might misinterpret “regular strength training” as needing heavy lifting, whereas body‑weight exercises can be equally effective for many. Fourteenth, the suggestion to pair cardio with two strength sessions weekly is solid, but the lack of guidance on periodization leaves novices uncertain about progression. Finally, the piece could have included a brief disclaimer about medication interactions, especially for those on statins, since exercise can sometimes exacerbate muscle‑related side effects. In sum, the article is a good starting point but would serve readers better with more nuance, acknowledgment of real‑world barriers, and a deeper dive into the interplay of lifestyle factors.
Look the results speak for themself – our bodies adapt when we movin around, no need for all that fancy diet crap. The statins are just a govt ploy to keep us in debt, just keep exercisin and you’ll be fine.
While I appreciate the drive for self‑reliance, it’s crucial to recognize that the physiological improvements from exercise can be dramatically blunted by chronic stress and poor sleep, factors that often accompany the very lifestyle changes we advocate. Moreover, asserting that “no need for fancy diet crap” overlooks the synergistic impact of nutrient timing and macronutrient composition on lipid metabolism. For instance, omega‑3 fatty acids have been shown to modestly raise HDL and even lower triglycerides, complementing the enzymatic pathways activated by physical activity. Ignoring these nuances can inadvertently set people up for disappointment when exercise alone doesn’t deliver the expected blood‑work results. A balanced approach, integrating both movement and thoughtful nutrition, tends to yield the most sustainable cardiovascular benefits.
Great article! If you’re just starting out, try adding a quick 5‑minute walk after each meal – it’s an easy way to boost daily activity without feeling overwhelmed.
What a fantastic guide! 🌈 I love how it blends science with practical steps – truly a rainbow of health! Remember, even a short jog can paint your arteries with brighter colors.
Absolutely, zaza! 🌟 Adding a splash of color to our workouts keeps motivation high. Try mixing in some dance moves – it’s fun and cranks up the heart rate while you groove to your favorite tune!
Honestly, I think the whole “exercise lowers cholesterol” hype is a bit overrated; sure, it helps a bit, but diet and meds still do the heavy lifting.
Hey everyone! 🙌 Let’s keep the vibes positive – even a 10‑minute jump rope session can spark those good‑cholesterol changes. Keep moving and smile!
The article is overly optimistic; real‑world results vary widely.
Don’t forget that every small step adds up – a brisk walk after dinner, climbing stairs, or a quick bike ride can collectively shift your cholesterol profile for the better.
Well said, Sruthi. It’s all about consistency, and even modest activity can make a difference over time.
Exercise is a moral duty to your heart; neglecting it is simply irresponsible.
The statement "regular movement not only burns calories" is missing a comma after "calories"; otherwise, the point is well made.