Anemia Management: Practical Steps to Treat Low Iron and Boost Energy
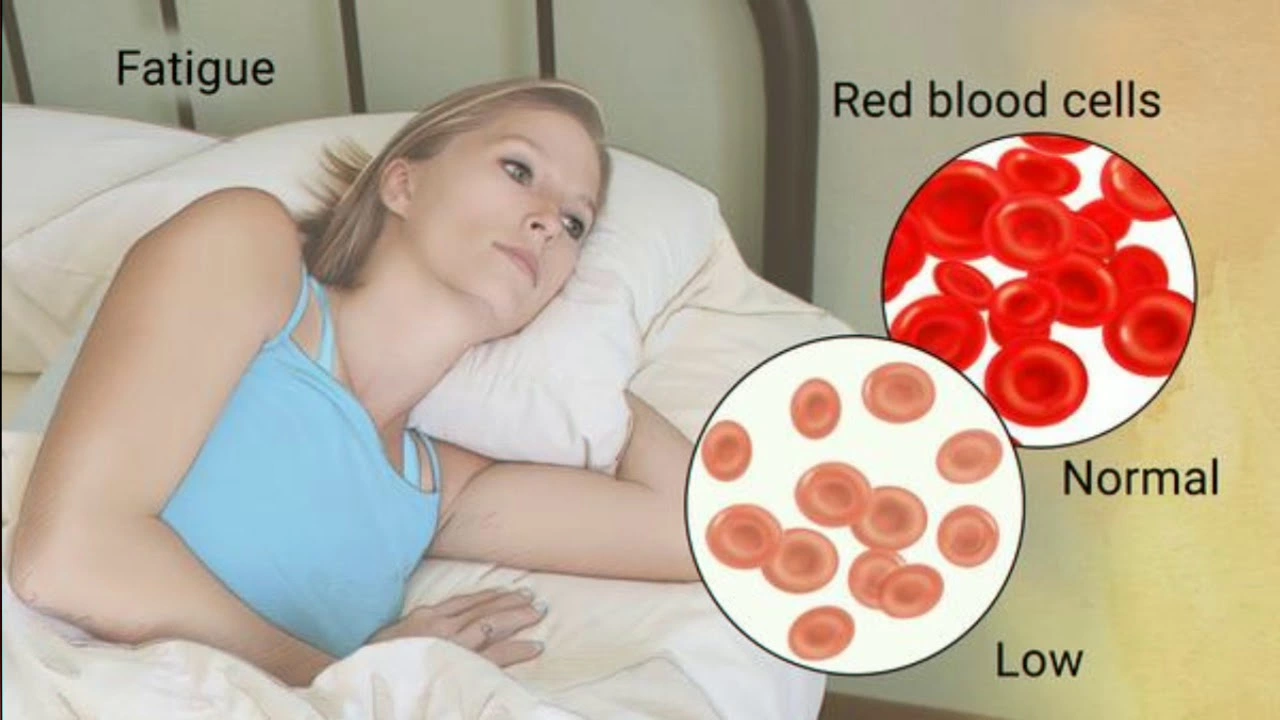
Feeling tired, short of breath, or just not yourself? Those are common signs of anemia — and many of them improve fast with the right steps. This page gives clear, usable advice on testing, diet, supplements, and when to get medical help.
Quick, useful checks and tests
First thing: get a CBC and ferritin. CBC tells how low your hemoglobin is; ferritin shows iron stores. Ask your doctor to also check B12 and folate if the CBC shows large red cells (high MCV). Stool tests or scopes may be needed if there’s unexplained bleeding. Knowing the cause of anemia is the most important step — treating symptoms alone often fails if the root problem keeps going.
If you have heavy periods, a history of ulcers, or stomach surgery, mention it. Pregnancy, chronic kidney disease, and some medications can cause anemia too. Track symptoms: dizziness, fast heartbeat with minimal exertion, pica (craving non-food items) — these help clinicians decide urgency and treatment.
Simple, practical ways to boost iron and blood health
Diet matters. Eat heme iron from meat, poultry, and fish — it’s absorbed best. Add vitamin C (citrus, peppers) to meals to help absorb non-heme iron from beans, lentils, spinach, and fortified cereal. Avoid drinking tea or coffee with meals; tannins cut iron absorption. Space calcium supplements and milk away from iron-rich meals.
For low iron, oral iron supplements are the usual start. Ferrous sulfate, gluconate, and fumarate are common. A typical goal is a dose that gives enough elemental iron (often around 60–65 mg elemental iron every other day can work well and reduces stomach upset). If tablets upset your stomach, try taking them with a light snack or switch to a different salt. Some people tolerate liquid iron better. Give oral iron time — hemoglobin often starts to rise in 2–4 weeks and stores take months to refill. Keep taking iron as your doctor recommends, even after symptoms improve.
If oral iron doesn’t work (intolerance, poor absorption, or very low levels), IV iron is fast and safe under medical supervision. People with kidney disease or undergoing chemo may get erythropoiesis-stimulating drugs. B12 injections are needed for true B12 deficiency — pills won’t fix severe deficiency quickly enough for some cases.
Practical tips: try every-other-day dosing to improve absorption and cut side effects; take vitamin C with iron; separate iron from calcium or antacids by 2–3 hours; keep follow-up blood tests every 4–8 weeks until stable.
Get urgent care if you have chest pain, fainting, severe shortness of breath, or very heavy bleeding. Otherwise, most people see gradual improvement with the right plan. Fixing the cause and following a simple, consistent treatment plan will get your energy back and protect your health long term.