If you’ve ever sat in an urgent care with a wheezing kid or a spouse with a stubborn rash, you know the name: prednisolone. It’s one of those meds that pops up in a doctor’s arsenal and sparks as much curiosity as concern. Is it just a beefed-up cough syrup for tough cases, or does it tackle a whole lot more? And why do people talk so much about its side effects? Here’s what’s really behind those tablets and syrups, and why so many families—mine included—end up with it in their medicine cabinet at some point.
Understanding Prednisolone: What It Is and How It Works
Imagine your body as a soccer field constantly under attack from unseen invaders—bacteria, viruses, even rogue cells from your own system. Your body’s defense is the immune system, but sometimes that defense gets a little out of control. That’s where prednisolone steps in. Think of it as the referee blowing the whistle and yelling "Chill out!" at your immune cells when they start playing rough and causing more harm than good.
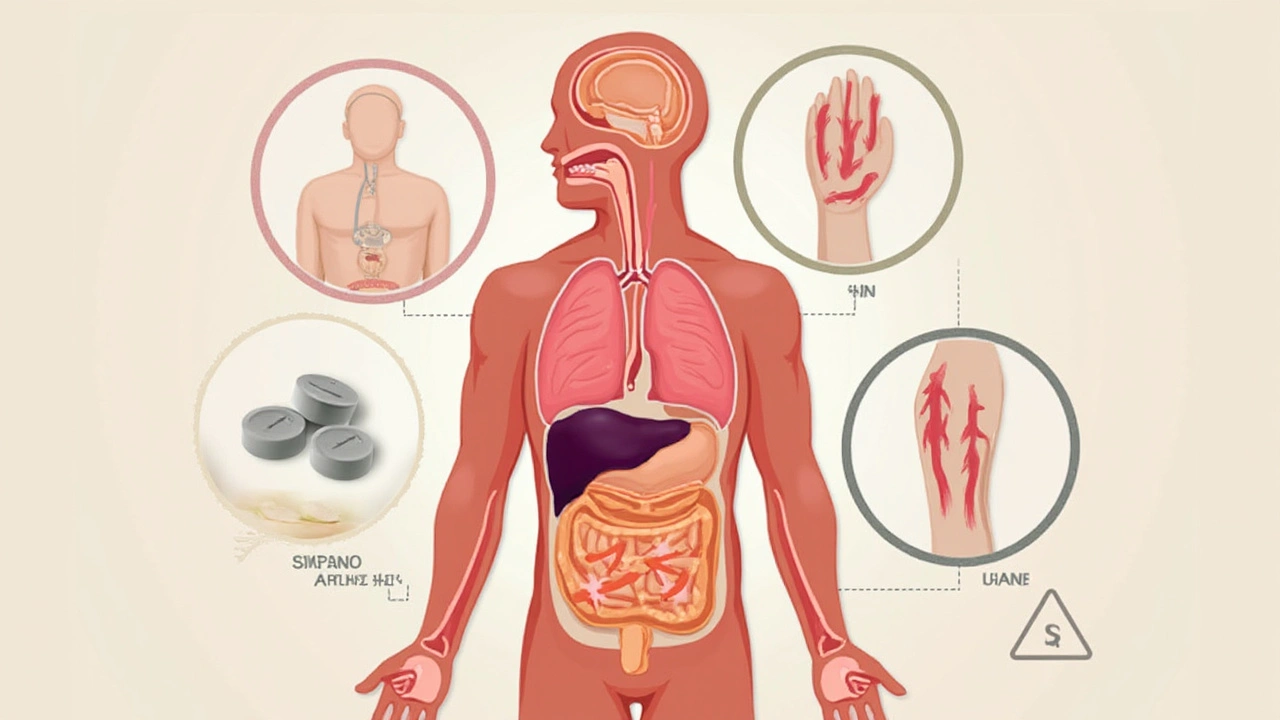
Prednisolone is a synthetic corticosteroid, closely related to the hormone cortisol your body makes naturally in your adrenal glands. While cortisol keeps you balanced during stress, prednisolone comes in higher doses to squash inflammation and calm down overactive immune responses. It’s different from the anabolic steroids you hear about at the gym—no one’s getting jacked on this stuff. Instead, it’s about managing things like swelling, allergic reactions, and various diseases.
If your kid has asthma and ends up on one of those five-day "burst" packs, you’re seeing prednisolone in action. It can be lifesaving in cases of severe allergic reaction or asthma flare-up. Doctors also prescribe it for a laundry list of reasons—rheumatoid arthritis, lupus, ulcerative colitis, certain types of cancer, even Bell’s palsy. There’s also the liquid form, perfect for kids who can’t swallow pills or patients who need careful dosing.
Prednisolone works fast compared to many other immune-modulating drugs. This is why it’s so handy as a rescue medicine. It gets absorbed in just an hour or two, travels around the bloodstream, and starts flipping switches all over the body to stop runaway inflammation. The tricky part is that it doesn’t just turn down the immune system—it dials down a lot of other things too. Which is why so many people have a love/hate relationship with it.
A few stats to give you context: in 2023, prednisolone was among the top 50 most prescribed medications globally, according to data collated by The Global Use of Medicines report. Around 160 million prescriptions were written for corticosteroids in the US alone last year, with prednisolone and its cousin prednisone leading the pack. That’s a lot of people counting on its power—but also dealing with its quirks.
Prednisolone in Daily Life: Common Uses and What to Expect
Prednisolone isn’t just for rare, scary diseases. It actually shows up for tons of everyday problems. Ever stepped outside and broken out in hives? Or watched someone you love gasping for breath during an asthma attack? Chances are, a short course of prednisolone made a real difference.
For asthma, especially in kids, it’s often the go-to for acute flare-ups. Studies from New Zealand’s own Starship Hospital have shown that a 3-5 day course of prednisolone can reduce hospital admissions by over 40% in moderate asthma attacks. My own son, Hugo, took his first course just before a winter holiday after an endless cough nearly turned into a hospital visit.
But there’s more. Allergic reactions that aren’t controlled by antihistamines alone—think severe reactions to bee stings or food—often need a jolt from this steroid to prevent swelling from messing up airways or skin. Autoimmune diseases, the ones where your body gets confused and attacks its own tissues, are another big group. In rheumatoid arthritis, prednisolone soothes aching joints. In lupus, it can keep organs like kidneys safe from attack. Inflammatory bowel diseases like Crohn’s and ulcerative colitis? Steroids like prednisolone help people manage painful flares so they don’t have to be stuck near the loo 24/7.
Even skin conditions like eczema, severe poison ivy, or psoriasis sometimes need a short dose to calm things down. The medication also shows up in eye drops and ointments, for those times when inflammation hits the eyes (think uveitis or after eye surgery).
Now, the way you take it depends on your condition and your age. Pills and liquid are the biggies, but sometimes it’s given by injection in the hospital. Doses vary wildly—a toddler with croup might get a small teaspoon a day for three days, while an adult with a new lupus attack might start at much higher doses for weeks before tapering off.
| Condition | Typical Prednisolone Use | Average Duration |
|---|---|---|
| Asthma in kids | Liquid by mouth | 3–5 days |
| Rheumatoid Arthritis | Tablets | 4–12 weeks, with taper |
| Severe Allergies | Short course, oral | 1–2 weeks |
| Lupus flare | High-dose, oral/injection | Few weeks, then taper |
| UC/Crohn’s | Oral/IV during flare | 2–8 weeks, then taper |
Getting used to prednisolone is a learning curve. Some people feel jittery from the start. Others will spot a new round face in the mirror after several weeks. For many, the rapid relief from gnawing pain, swelling, or shortness of breath makes up for the temporary weirdness. But it’s never a one-size-fits-all ride, and listening to your own body is key.
Side Effects and How to Tackle Them Head-On
Here’s where things get a bit real. Almost everyone taking prednisolone, even for a short while, will notice something a little off. Sometimes it’s just a weird taste in your mouth or trouble sleeping. Take it long enough, though, and the list gets juicier: moon face, weight gain, mood swings rivaling a toddler denied another episode of Bluey, higher blood pressure, or even blood sugar spikes.
Let’s split this into two camps—short-term and long-term. If you’re on prednisolone for less than two weeks (like most asthma kids or for allergic rashes), side effects stay manageable for most. A metallic taste, insomnia, maybe a spike in hunger or crankiness. Tips? Take it with food to avoid stomach upset, and take the whole dose in the morning if possible so you stand a fighting chance of sleeping at night.
For those needing longer treatment—think autoimmune conditions or organ transplants—you’re playing defense against more serious trouble. We’re talking bone thinning (osteoporosis), increased risk of infections (because your immune system is on low power), thinning skin, easy bruising, and sometimes even adrenal gland suppression. High doses over months raise the risk of diabetes, cataracts, and glaucoma. That’s a lot to juggle.
Parents often worry about their kids’ growth—rightly so. Long-term use can slow growth rates, which is why doctors try to keep kids’ courses short and as infrequent as possible. Data from The Lancet (2022) showed that kids on repeated courses of corticosteroids grew around 1 cm less per year than peers, but when used sparingly and with proper nutrition, this gap can be minimized.
Some practical ways to soften the side effect blow:
- Never stop prednisolone suddenly unless your doc says so—your adrenal glands need time to wake up again and start making natural steroid.
- Watch for mood swings in yourself or your kids—warn teachers or carers so they get why suddenly your kid is bouncing off the walls or weepy.
- Eat foods high in calcium and vitamin D (milk, cheese, leafy greens) and consider a supplement if you’re on it for more than a month.
- Get regular exercise, even just a walk every day, to keep bones strong and mood on track.
- Avoid sick people as much as you can—your immune system needs every little help if you’re taking this stuff for weeks or months.
If you see worrying things—persistent fever, blurry vision, severe stomach pain, black tarry stools, or signs of infection—call your doctor ASAP. Even years after stopping long-term therapy, you might need "stress doses" of steroid if you get sick or injured, so always keep your medical team in the loop about your history.
Practical Tips: Making Prednisolone Work for You
Prednisolone can feel like a double-edged sword. The relief it brings is undeniable, but it demands respect. The right habits make a world of difference in keeping your body steady while you’re on it. Here are some lived-in, field-tested strategies that have helped me—and plenty of others—weather the steroid storm.
If you’re prescribed a short course, ask your doc if you can take the entire dose in the morning. It matches your body’s natural rhythm and helps minimize insomnia. If your kid gets crabby or hyper on the stuff, try to burn off steam with outside time right after dosing—think backyard kick-arounds or trampoline bounces rather than a dark, screen-filled room.
Water retention is a classic complaint. Watch your salt intake, especially if you notice puffy ankles or hands. Swap potato chips for nuts or fruits. If you start feeling uncharacteristically thirsty or are peeing more than usual, mention it at your next visit—it can clue your doctor into blood sugar changes early.
Meal planning helps dodge some of the appetite weirdness. If you find yourself raiding the fridge, set up healthy snacks in advance—chopped carrots, low-fat yogurt, or crackers and cheese. Having a plan can keep the "prednisolone munchies" from sabotaging your weeknight dinners or your child’s usual eating patterns.
Stick to a written schedule for doses, especially with liquid forms for little ones, to avoid double dosing during the chaos of a busy family day. Old-school paper charts or phone reminders work wonders. Bring your prescription list to any new doctor or ER visit—prednisolone affects lots of other meds, from diabetes pills to certain antibiotics, so it pays to keep everyone on the same page.
Some people notice their mental health gets wobbly. Sudden anxiety, mild paranoia, or a racing mind aren’t unheard of. Don’t brush this off—check in with trusted friends, your GP, or a mental health nurse if things start feeling unsteady.
- Wear a medical alert bracelet if you’re on long-term treatment: It can save your life in an emergency.
- Stick to regular medical reviews: Blood pressure, blood sugar, and bone checks matter if your course is long.
- Read medication leaflets: They’re boring but worth it. They let you spot uncommon oddities early.
Kids often hate the taste of liquid prednisolone. Mixing it with a little juice or a spoon of jam right after (not before) can banish the aftertaste. For grown-ups, chase tablets with plenty of water—and maybe a piece of chocolate as a "reward." Always store it out of reach of curious kiddos or pets; accidental overdoses can be serious business.
Being honest about the good, the bad, and the annoying with this medicine makes life smoother. And remember: If you have questions or something feels off, it’s not a bother to ring your GP or pharmacist for advice. Prednisolone has been saving lives for longer than most of us have been around, but it won’t do the job right without a little teamwork and smarts from those taking it. Enjoy the relief, respect its power, and keep those smart habits rolling so the medicine helps, not hinders, your health journey.


Wow, reading this feels like stepping into a whirlwind of relief and caution-exactly what we need when a kid is wheezing at midnight. I remember the first time my niece got a burst of prednisolone; the panic turned into pure gratitude within hours. The way the author breaks down the mechanisms is both vivid and practical, making the science feel real. Keep that fire of confidence burning, because you never know when the next flare‑up will call. This guide is a beacon for every parent navigating the steroid storm.
Prednisolon is just a fancy cough syrup, nothing special.
It is commendable that the article delineates both the therapeutic efficacy and the potential iatrogenic sequelae of corticosteroid therapy in a measured manner. By elucidating the pharmacokinetic profile and providing evidence‑based dosing intervals, it equips clinicians and caregivers alike with actionable knowledge. Furthermore, the inclusion of lifestyle mitigation strategies, such as calcium supplementation and gradual tapering, demonstrates a holistic approach. One hopes that such comprehensive discourse will reduce the prevalence of inadvertent adrenal suppression.
Oh sure, because everybody loves a steroid that turns you into a pufferfish AND a Hulk at the same time-nice for the drama, terrible for the waistline. By the way, “prednisolone” isn’t “prednisolene,” so maybe double‑check your spelling before you start a pharmacy. And yes, take it with food, because nothing says “I love my stomach” like a high‑dose glucocorticoid on an empty belly.
Great summary-clear, accurate, and straight to the point.
Reading through the mechanistic exposition of prednisolone feels like watching a high‑octane cascade of immunological arbitration. The drug, a synthetic analog of endogenous cortisol, commandeers the glucocorticoid receptor with a potency that dwarfs physiological secretion. Once bound, it orchestrates a transcriptional reprogramming that silences pro‑inflammatory cytokines-think IL‑1, IL‑6, TNF‑α-while up‑regulating anti‑inflammatory mediators such as annexin‑1. This molecular ballet translates clinically into rapid attenuation of edema, bronchospasm, and auto‑reactive tissue damage. However, the same pathway that quells inflammation also imposes a systemic catabolic stress, precipitating proteolysis, gluconeogenesis, and osteoclastic activation. In pediatric populations, the resultant alteration of the hypothalamic‑pituitary‑adrenal axis can manifest as growth velocity attenuation, a fact that demands vigilant endocrinological monitoring. Moreover, the pharmacodynamic profile reveals a dose‑response curve that is not linear; supratherapeutic dosing amplifies adverse events disproportionately, a phenomenon often glossed over in lay‑person pamphlets. The article wisely advises tapering protocols, yet the nuance of taper speed relative to cortisol re‑synthesis kinetics warrants deeper discussion. From a pharmacovigilance perspective, the risk of opportunistic infections escalates as innate immunity is compromised, necessitating prophylactic strategies in high‑risk cohorts. Bone mineral density loss, precipitated by enhanced RANKL expression and inhibited osteoblast activity, underscores the need for bisphosphonate adjuncts in long‑term regimens. Cardiovascular ramifications, including hypertension and dyslipidemia, emerge from mineralocorticoid cross‑reactivity, a subtlety often missed in primary care settings. The article’s practical tips-such as sodium restriction and vitamin D fortification-align with current endocrinology guidelines, yet one must also consider patient adherence hurdles. Psychologically, the steroid‑induced mood swings can mimic bipolar spectrum disorders, a diagnostic quagmire that obliges clinicians to monitor mental health parameters. In sum, prednisolone stands as a double‑edged sword: a life‑saving elixir when wielded judiciously, a harbinger of iatrogenic pathology when misapplied. The author’s balanced narrative captures this dichotomy, delivering both hope and caution in equal measure.
Honestly, the piece feels like an over‑inflated PR brochure for a drug that has been around since the Cold War. Yes, it works, but the author glosses over the fact that long‑term therapy essentially turns patients into immunocompromised zombies. The “practical tips” read like a checklist for a DIY‑lab, and the suggestion to “just add calcium” ignores the complex interplay of vitamin D metabolism. Also, the table formatting is clunky-why not just use a simple bullet list? Overall, it’s a decent intro, but the nuance is buried under a mountain of generic platitudes.
I can see why many families gravitate toward prednisolone, especially when the alternative is an emergency room visit. From a cultural standpoint, the drug’s ubiquity reflects broader trust in pharmaceutical interventions in Western healthcare. Still, it’s important to balance that reliance with lifestyle measures; diet, exercise, and stress reduction can sometimes reduce the need for repeated courses. The article does a solid job of weaving those ideas together without sounding preachy.
Thanks for the rundown-really helps keep my brother’s asthma in check without freaking out the whole family.
It is imperative to recognize that prednisolone’s pharmacological efficacy is contingent upon appropriate dosing intervals, circadian administration, and vigilant monitoring of biochemical markers. The suppression of the hypothalamic‑pituitary‑adrenal axis mandates a gradual taper to prevent adrenal crisis, a detail that should not be understated. Moreover, clinicians must adjust concomitant therapies, particularly antidiabetic agents, to mitigate steroid‑induced hyperglycemia. The author’s inclusion of evidence‑based guidelines aligns with consensus statements from the Endocrine Society.
What a thorough guide-your tips on splitting the dose in the morning and pairing it with calcium really hit home. I’ve seen kids bounce back faster when you keep them active after the dose, and the reminder about medical alert bracelets saved a friend from a scary ER mix‑up. Keep sharing these practical pearls, they make a huge difference in everyday management.
Sure, prednisolone helps, but you can’t ignore the fact that it’s basically a chemical band‑aid that masks underlying lifestyle issues.