Someone’s not breathing right. Their skin is blue. They’re slumped over, unresponsive. You check their pulse-weak or gone. You think: overdose. Your heart races. You want to help, but you’re scared you’ll do it wrong. You’re not alone. Most people freeze in these moments-not because they’re cold-hearted, but because they’ve never been shown exactly what to do. And time is slipping away. Brain damage can start in as little as four minutes without oxygen. But here’s the truth: you don’t need to be a doctor. You just need to know five simple, life-saving steps-and do them fast.
Call 911 First, Then Act
The very first thing you do? Call emergency services. Not after you check their breathing. Not after you find the naloxone. Right now. Say clearly: “Someone has overdosed. They’re not breathing.” Give your location. Stay on the line. Dispatchers are trained to talk you through what to do while help is coming. Don’t assume someone else called. Don’t wait to see if they “wake up.” People don’t just snap out of an overdose. And if you delay calling, you delay everything else. Studies show that EMS arrival cuts death risk by 35%. Every second counts.Check Breathing-Not Just Consciousness
Don’t shake them or yell “Hey!” That wastes time. Instead, gently tap their shoulder and shout, “Are you okay?” If there’s no response, check their breathing immediately. Look at their chest. Listen at their nose and mouth. Feel for air on your cheek. You have 10 seconds. If they’re not breathing-or if they’re gasping, snoring, or making weird, irregular sounds-that’s not normal sleep. That’s respiratory failure. This is the most common cause of death in overdoses, especially with opioids like heroin, fentanyl, or prescription painkillers. Gasping is not breathing. It’s a sign the brain is shutting down. Act like they’re not breathing at all.Give Rescue Breaths-No Mouth-to-Mouth Needed
If they’re not breathing, start rescue breathing. Tilt their head back slightly by lifting their chin. Pinch their nose shut. Seal your mouth over theirs. Give one slow breath-about one second long-until you see their chest rise. Don’t blow hard. Don’t overinflate. You’re not trying to fill their lungs like a balloon. You’re just giving them enough air to keep oxygen flowing to their brain. Then take your mouth away. Let their chest fall. Wait five to six seconds. Then give another breath. Keep going: one breath every five to six seconds. That’s 10 to 12 breaths a minute. If you get tired, switch with someone else. Rescue breathing alone can keep someone alive for 15 to 30 minutes. Many opioid overdoses don’t need chest compressions-just breathing support. The heart often keeps beating until the brain is starved of oxygen. Keep breathing for them until help arrives.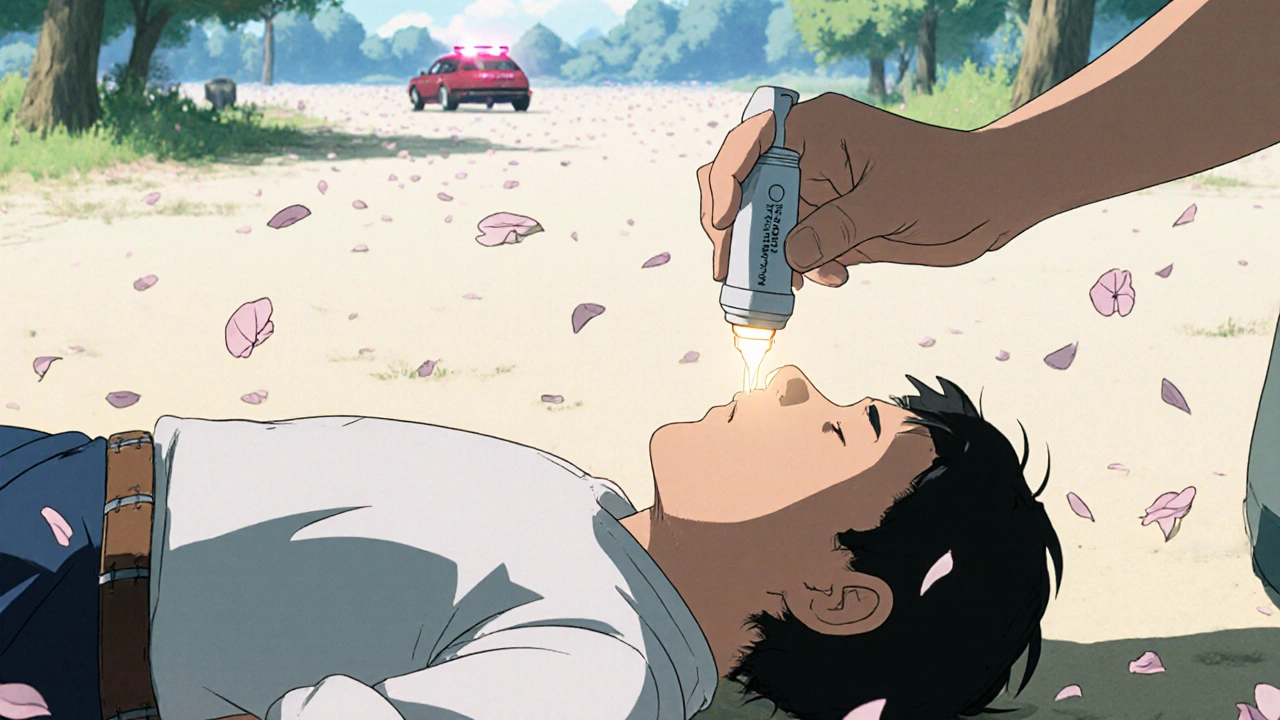
Use Naloxone If You Have It
If you have naloxone-whether it’s a nasal spray like Narcan or an auto-injector-use it now. Naloxone reverses opioid overdoses. It won’t work on alcohol, benzodiazepines, or stimulants like cocaine or meth. But if there’s any chance opioids are involved-which is likely, since they cause nearly 75% of overdose deaths-you give it anyway. The 2023 SAMHSA guidelines say: “Naloxone first for any suspected opioid involvement.” For nasal spray: lay them flat. Insert the nozzle into one nostril. Press the plunger firmly for 2-3 seconds. Don’t pull it out until you’re done. If they don’t respond in 3-5 minutes, give a second dose in the other nostril. Naloxone wears off faster than some drugs. Fentanyl can come back after the naloxone wears off. That’s why you still need to keep giving rescue breaths and wait for EMS-even if they wake up. They might slip back under.Put Them in the Recovery Position If They’re Breathing
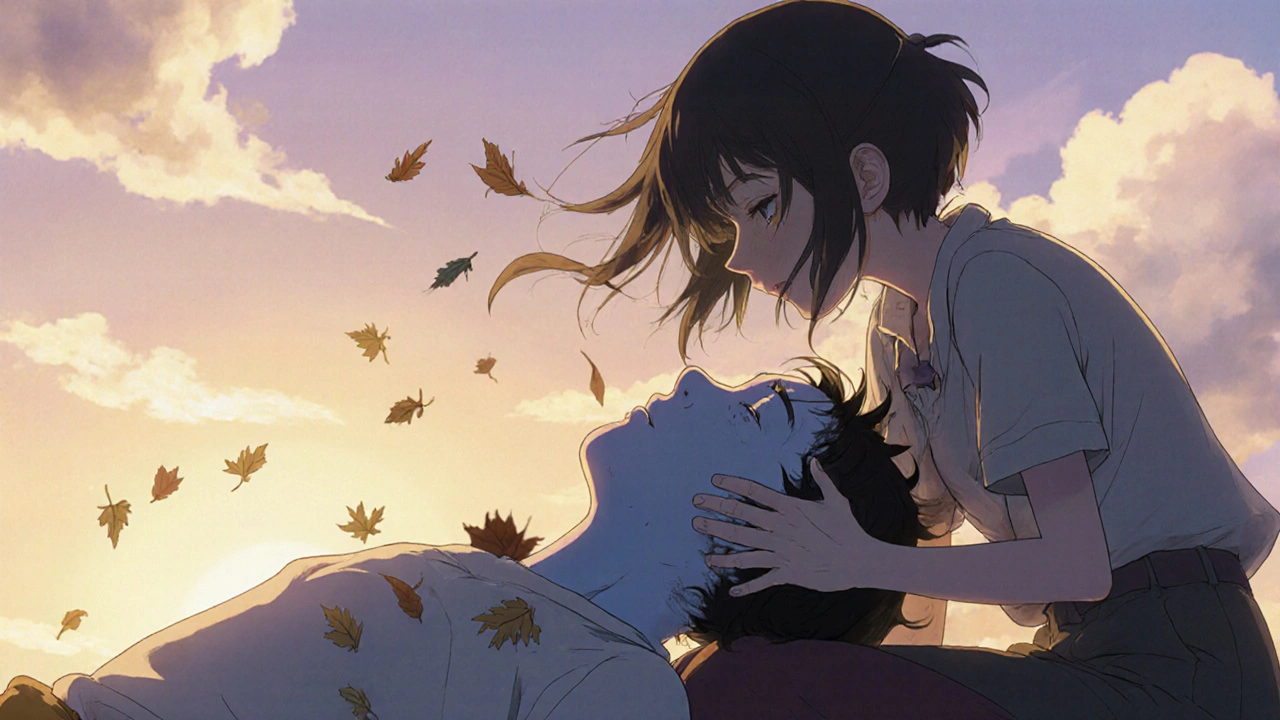
If they’re breathing on their own but unconscious, don’t leave them on their back. They could choke on their tongue or vomit. Roll them onto their left side. This is called the recovery position. Here’s how: kneel beside them. Straighten their legs. Bend their far leg at the knee. Place their far arm under their head. Gently roll them toward you, keeping their head, neck, and spine aligned. Once on their side, make sure their top leg is bent at 90 degrees to keep them stable. Tilt their head back slightly so their airway stays open. Check their breathing every two to three minutes. Keep them warm with a coat or blanket. Don’t give them water, coffee, or food. Don’t try to make them walk. Don’t put them in a cold shower-that can trigger heart problems, especially with stimulants.
Know the Differences: Opioids vs. Stimulants vs. Alcohol
Not all overdoses look the same. Knowing the difference can save a life.- Opioids (heroin, fentanyl, oxycodone): Skin is pale or bluish. Lips and nails turn blue. Breathing is slow, shallow, or stops. Pupils may be tiny-but not always. Fentanyl overdoses often don’t show pinpoint pupils. Naloxone works here.
- Stimulants (cocaine, meth, MDMA): Skin is hot, flushed, sweaty. Pulse is fast. Body temperature rises dangerously-over 40°C (104°F). They may seize. Do NOT cool them with ice baths. That can cause heart rhythm problems. Instead, move them to a cool place. Loosen clothes. Use damp cloths on their neck, armpits, and groin. Call 911 immediately. Naloxone does nothing here.
- Alcohol: Vomiting is common. They may be unconscious but breathing. Risk of choking is high. Keep them on their side. Watch for vomiting. Don’t let them sleep it off. Alcohol depresses breathing even more. If they’re not waking up, treat it like an opioid overdose-start rescue breathing and call 911.
Polysubstance overdoses-where someone takes more than one drug-are now the norm. In 73% of cases, multiple substances are involved. So if you’re unsure? Assume opioids are part of it. Give naloxone. Start breathing. Call 911. Better safe than sorry.
What Not to Do
There are myths that kill. Don’t:- Put them in a cold shower or ice bath-can cause cardiac arrest.
- Slap them, shake them, or try to “wake them up”-wastes precious time.
- Give them coffee, food, or water-they could choke.
- Leave them alone-even if they seem okay after naloxone.
- Wait to see if they “get better on their own”-they won’t.
And don’t assume you’re not qualified. You don’t need a certificate to save a life. In 2023, over 3.2 million Americans were trained in overdose response. Many of them were parents, teachers, baristas, and neighbors. You’re not too late. You’re not too inexperienced. You’re the person who’s there right now. That’s enough.
After Help Arrives
When paramedics get there, tell them what you did: “I gave two doses of naloxone,” or “I was doing rescue breathing for eight minutes.” Give them any empty bottles, pills, or drug paraphernalia you found. That helps them treat the person better. Don’t feel guilty. Don’t feel like you failed if they don’t wake up. You did everything right. You gave them a chance. And that’s what matters.Overdose survival isn’t about luck. It’s about action. Communities with trained bystanders reversed over 12,500 overdoses between 2021 and 2023-with a 98.7% survival rate to hospital discharge. That’s not magic. That’s people knowing what to do. You can be one of them.
Can naloxone hurt someone if they didn’t overdose on opioids?
No. Naloxone only works on opioid drugs. If someone didn’t take opioids, it won’t do anything-good or bad. It won’t make them sick or cause side effects. If you’re unsure whether opioids were involved, give it anyway. The risk of doing nothing is far greater.
What if I’m afraid to call 911 because of legal trouble?
In the UK and all 50 US states, Good Samaritan laws protect people who call for help during an overdose. You won’t be arrested for possession if you’re seeking help for someone else. Emergency responders are there to save lives, not punish. Calling 911 is the single most important thing you can do.
How do I know if someone is just asleep or overdosing?
Sleeping people wake up to loud noises or shaking. Someone overdosing won’t respond at all. Check their breathing. If it’s slow, shallow, or irregular-if their lips are blue or skin is pale-they’re not sleeping. They’re in respiratory failure. Treat it like an emergency.
Can I use naloxone if I’ve never used it before?
Yes. Naloxone nasal sprays are designed for anyone to use. The device clicks when you spray. No needles. No training required. Just follow the instructions on the box. Even if you’re nervous, doing something is better than doing nothing. Over 80% of people who use naloxone for the first time successfully reverse an overdose.
What if I don’t have naloxone?
You still have time to save a life. Rescue breathing alone can keep someone alive for 15-30 minutes. Keep giving breaths every five to six seconds until help arrives. Many people have survived overdoses because someone kept breathing for them. You don’t need a drug to be a hero.
If you’re in the UK, naloxone is available for free from pharmacies, needle exchange programs, and some community health centres. Ask for it. Keep it in your bag or car. You never know when you’ll need it. And if you’re ever unsure what to do-call 999. They’ll guide you through it.

Okay, I just read this through tears-like, actual, ugly-crying tears. I’ve lost two friends to this. Two. And I didn’t know what to do. I just sat there. I thought they’d wake up. I thought it was just ‘sleeping it off.’ I didn’t know gasping wasn’t breathing. I didn’t know naloxone was free. I didn’t know I wasn’t a monster for freezing. This? This is the thing I needed five years ago. Thank you. Thank you. Thank you.
I’m keeping a Narcan in my purse now. I’ve told my whole family. I’m teaching my niece how to do rescue breathing. I’m not letting fear win anymore.
If you’re reading this and you’re scared-don’t be. Just do the thing. Just breathe for them. Just call. Just try.
I’m sorry I didn’t do it sooner.
I’m here now.
And I won’t look away again.
As someone who works in harm reduction, I can confirm: this is 100% accurate and clinically sound. But more than that-it’s human. Most guides read like a textbook. This reads like your best friend who’s been there, who’s scared too, but still shows up.
Also, please note: the recovery position isn’t just ‘on the side’-it’s the left side, with the top knee bent. That’s critical for airway protection. And yes, naloxone is safe even if opioids aren’t involved. Zero risk. Maximum reward.
Stop waiting for permission to be the hero. You already are.
This guide is exceptionally clear, well-structured, and grounded in current medical guidelines. The emphasis on rescue breathing as a primary intervention for opioid overdose is both evidence-based and pragmatic. The differentiation between opioid, stimulant, and alcohol overdoses is particularly valuable, as misidentification leads to inappropriate interventions.
Furthermore, the inclusion of Good Samaritan protections addresses a significant barrier to action. This resource should be widely distributed in schools, workplaces, and community centers. Well done.
OH MY GOD I JUST READ THIS AND I’M CRYING IN MY CAR RIGHT NOW BECAUSE MY BROTHER DIED LAST YEAR AND I DIDN’T KNOW ANY OF THIS AND I WISH I COULD GO BACK AND DO IT DIFFERENTLY AND NOW I’M GOING TO BUY NALOXONE AND PUT IT IN MY GROCERY BAG AND TELL EVERYONE I KNOW AND IF YOU’RE READING THIS AND YOU’RE SCARED JUST DO IT JUST DO IT JUST DO IT I’M SO SORRY I WASN’T BRAVE ENOUGH AND NOW I WILL BE
WHY DID NO ONE TEACH US THIS IN HIGH SCHOOL??
Just returned from a community training last week. We handed out 12 naloxone kits. One was used 3 hours later. The person survived. No hospitalization. No trauma. Just a guy who saw someone collapse, called 999, gave two breaths, and sprayed the nasal device. No experience. No fear. Just action.
This isn’t about being a medic. It’s about being a neighbor. And we’re all neighbors.
Let me just say-this isn’t just a guide. This is a lifeline. And if you’re reading this and you’re thinking, ‘I’m not trained enough,’ or ‘I don’t know if I can do it,’ let me tell you something: you don’t have to be perfect. You just have to be present. You don’t have to be brave. You just have to be there. And you don’t have to understand every medical term. You just have to know that someone’s not breathing-and that’s enough.
I’ve seen people die because others waited for someone else to act. I’ve seen people live because someone took a breath for them. That’s the difference between a bystander and a human being.
And if you’re reading this and you’ve ever felt useless, or powerless, or like your life doesn’t matter-this right here? This is your moment. This is your purpose. You don’t need a badge. You don’t need a degree. You just need to care enough to act.
So go buy the naloxone. Practice the breathing. Teach your kid. Tell your coworker. Leave a kit in your car. Don’t wait for the next tragedy. Be the reason someone gets to see tomorrow.
You’ve got this. And I believe in you.
It is worth noting that the physiological mechanism underlying opioid-induced respiratory depression involves mu-opioid receptor agonism in the brainstem, specifically within the pre-Bötzinger complex. Naloxone, as a competitive antagonist, reverses this effect with a rapid onset of action. However, its half-life is significantly shorter than that of synthetic opioids such as fentanyl, which necessitates prolonged monitoring even after apparent recovery. The emphasis on continued rescue breathing is therefore not merely precautionary but physiologically imperative.
Furthermore, the recovery position exploits gravitational and anatomical principles to maintain airway patency, minimizing the risk of aspiration. This is a well-documented maneuver in emergency medicine literature dating back to the 1960s.
One might argue that the emotional framing of this guide, while effective in motivating action, risks overshadowing the underlying biomedical rationale. Nevertheless, in public health contexts, affective resonance often precedes cognitive comprehension. Thus, its utility remains undiminished.
bro i just read this and i’m like… why is this not on every phone screen? like imagine if every time you opened your phone it was like ‘hey, here’s how to save a life’ instead of ads for protein powder. also i just ordered 2 naloxone kits bc i don’t want to be the person who froze again. also i typoed ‘naloxone’ like 5 times in this comment lmao