Introduction to Aspirin and COPD
As a blogger who focuses on health and wellness, I am always on the lookout for new and innovative treatments for various conditions. One such condition that affects millions of people worldwide is Chronic Obstructive Pulmonary Disease (COPD). COPD is a progressive lung disease that causes breathing difficulties, and it is primarily caused by smoking or long-term exposure to irritants in the air. In this article, we will explore the potential benefits of using aspirin as a treatment for those with COPD.
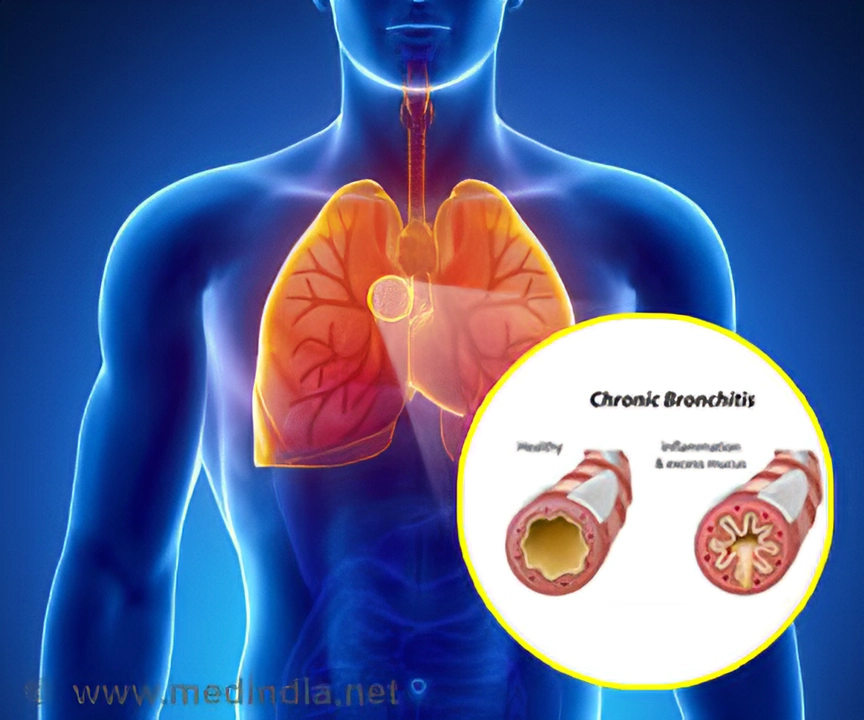
Understanding COPD: Symptoms and Causes
Before diving into the discussion about aspirin and COPD, it is essential to understand the symptoms and causes of this lung disease. Common symptoms of COPD include shortness of breath, wheezing, chronic cough, and frequent respiratory infections. The primary cause of COPD is smoking, but other factors such as air pollution, chemical fumes, and dust can also contribute to the development of the disease. COPD is a chronic condition, meaning that it worsens over time and can lead to severe health complications if not properly managed.
The Role of Inflammation in COPD
One of the main factors contributing to the progression of COPD is inflammation. Inflammation in the airways and lungs causes the walls of the airways to thicken, which in turn leads to a narrowing of the passages and reduced airflow. This inflammation is triggered by various factors, including exposure to irritants and the body's immune response to infections. Reducing inflammation is a crucial aspect of managing COPD and improving lung function.
Aspirin: A Potent Anti-Inflammatory
Aspirin is a well-known and widely used medication for its pain-relieving and anti-inflammatory properties. It works by inhibiting the production of prostaglandins, which are chemicals responsible for causing inflammation and pain. Due to its anti-inflammatory effects, aspirin has been studied for its potential use in the treatment of various inflammatory conditions, including COPD.
Research on Aspirin and COPD
Several studies have been conducted to examine the potential benefits of aspirin in COPD patients. Some of these studies have shown promising results, suggesting that regular aspirin use may help reduce the frequency of COPD exacerbations, improve lung function, and decrease the risk of hospitalization. However, it is important to note that not all studies have yielded positive results, and more research is needed to establish a definitive link between aspirin use and improved COPD outcomes.
Aspirin as a Preventative Measure
While the effectiveness of aspirin as a treatment for existing COPD is still under investigation, there is evidence to suggest that regular aspirin use may help prevent the development of COPD in individuals who are at risk. A study published in the American Journal of Respiratory and Critical Care Medicine found that long-term aspirin use was associated with a lower risk of developing COPD among smokers. This finding suggests that aspirin may have a protective effect on the lungs and help prevent the onset of COPD in susceptible individuals.
Potential Side Effects and Risks of Aspirin Use
As with any medication, aspirin use comes with potential side effects and risks. Some of the most common side effects of aspirin include gastrointestinal issues such as stomach pain, heartburn, and nausea. More serious risks of aspirin use include an increased risk of bleeding, ulcers, and allergic reactions. It is essential to discuss these risks with a healthcare professional before starting a regular aspirin regimen, especially for those with COPD or other chronic illnesses.
Consulting a Healthcare Professional
While the use of aspirin as a treatment or preventative measure for COPD is promising, it is essential to consult a healthcare professional before making any changes to your current treatment plan. Your doctor will be able to assess your individual needs and determine whether adding aspirin to your regimen is appropriate. They will also be able to closely monitor your progress and adjust your treatment plan as necessary to ensure the best possible outcomes for your health.
Conclusion
In conclusion, aspirin may offer potential benefits for those with COPD or individuals at risk of developing the disease. Its anti-inflammatory properties could help reduce inflammation in the lungs, improve lung function, and decrease the risk of COPD exacerbations. However, more research is needed to fully understand the relationship between aspirin and COPD, and it is vital to consult a healthcare professional before making any changes to your treatment plan. As always, the best way to manage COPD and maintain optimal lung health is to follow your doctor's recommendations, adhere to prescribed medications, and make necessary lifestyle adjustments such as quitting smoking and avoiding exposure to irritants.

Well, congratulations on discovering that aspirin, the age‑old kitchen‑cabinet staple, might have a role in COPD management. One might think the mere fact that it reduces prostaglandin synthesis instantly transforms it into a miracle cure, but alas, medicine rarely works that way. Still, kudos for shining a light on the anti‑inflammatory angle – it’s *almost* as exciting as a tie‑dye shirt at a funeral. Keep the optimism flowing; perhaps the next study will finally prove that a daily aspirin can replace inhalers. If nothing else, it gives your doctor something else to write on the prescription pad.
yo i read the whole thing and tbh i think the idea of using aspirin for copd is kinda wild but also kinda logical if u think about inflammation being the main villain – because, you know, aspirin’s been fighting pain since forever. i guess the data is still fuzzy, lol. but seriously, it could be a cheap add‑on if you’re already on it for heart health, maybe. lets just hope the researchers dont mess up the dosage and cause more gut pain.
Well, that's just common sense wrapped in a blog post.
I must say, the notion of repurposing a centuries‑old analgesic for a complex pulmonary pathology is, at the very least, an intellectually stimulating proposition.
Your exposition traverses the historical context of salicylates with commendable thoroughness.
However, one cannot overlook the pharmacodynamic caveats that accompany systemic cyclooxygenase inhibition in a population already predisposed to cardiovascular fragility.
Moreover, the heterogeneity of COPD phenotypes-emphysematous versus chronic bronchitic-demands a nuanced approach that a blanket antiplatelet strategy may simply not satisfy.
In clinical practice, we routinely balance the antithrombotic benefits of aspirin against its gastrointestinal toxicity, a calculus that becomes even more intricate when inhaled corticosteroids are in the therapeutic regimen.
It is also worth mentioning that the anti‑inflammatory potency of low‑dose aspirin pales in comparison to that of inhaled corticosteroids, which remain the cornerstone of exacerbation prophylaxis.
Nevertheless, the epidemiological signal you cite-namely, a reduced incidence of COPD among long‑term aspirin users-merits rigorous scrutiny, preferably through randomized controlled trials.
Such trials should stratify participants by smoking status, baseline inflammatory markers, and comorbidities, thereby elucidating any differential effect size.
One might also contemplate the role of aspirin’s irreversible platelet inhibition in modulating microvascular inflammation within the pulmonary circulation.
If a definitive benefit were established, the cost‑effectiveness of a readily available tablet could indeed revolutionize management algorithms.
Conversely, the potential for increased bleeding risk, especially in the context of concomitant anticoagulant therapy, cannot be dismissed lightly.
Therefore, a multidisciplinary dialogue encompassing pulmonologists, cardiologists, and gastroenterologists would be essential before any guideline endorsement.
In the interim, clinicians should continue to adhere to evidence‑based inhaled therapies while remaining vigilant for emerging data.
Your article, while optimistic, should perhaps temper its conclusions with a reminder of the current evidence hierarchy.
In sum, aspirin may hold promise, but it remains a hypothesis awaiting validation.
Until then, let us not abandon tried‑and‑true treatments in favor of speculative adjuncts.
I can't help but wonder who's really pulling the strings behind these 'clinical trials'. The pharma giants love to push cheap drugs like aspirin as a distraction while they line their pockets with newer, patented compounds. It's almost as if the entire narrative is crafted to keep us dependent on the healthcare system. Remember, every time you read about a 'breakthrough', ask yourself who's benefiting.
Wow, this is like the most exxtraordinary thing I've read all day!! I mean, aspirin for COPD? That's like saying you can fix a leaky roof with a band-aid!!! The drama of scientists trying to play doctor with a pill that's been around since the Roman empire is just too much. But seriously, the side effects could turn your life into a horror movie, and no one wants that. Keep an eye on those bleeding risks, folks!!!
From a pathophysiological standpoint, the modulation of cyclooxygenase pathways by acetylsalicylic acid could theoretically attenuate neutrophilic infiltrates in the bronchial mucosa, thereby reducing exacerbation frequency. However, the pharmacokinetic profile of low‑dose aspirin-characterized by rapid hepatic first‑pass metabolism and limited pulmonary bioavailability-raises questions about its efficacy as a monotherapy in COPD management. Clinical implementation would require robust biomarker stratification, perhaps leveraging sputum eosinophil counts or exhaled nitric oxide levels to identify responders. In practice, integrating aspirin into existing regimens must be done cautiously, with vigilant monitoring for gastrointestinal adverse events, especially in patients on concurrent anticoagulants. Ultimately, while the concept is intriguing, the evidence base remains preliminary, and further phase‑III trials are indispensable before any paradigm shift occurs.